What Is the Difference Between Cardioversion and Defibrillation
The real difference between cardioversion and defibrillation boils down to one simple question: does the patient have a pulse?
Cardioversion is what you turn to for a patient with a pulse who’s stuck in an unstable, dangerously fast heart rhythm. It's a controlled, synchronized electrical shock. Think of it like this: it’s a precise, timed reset button.
On the flip side, defibrillation is an all-out emergency intervention. This is for the patient in full cardiac arrest—no pulse, unresponsive. You deliver a powerful, unsynchronized shock to stop the chaotic electrical storm in their heart.
Distinguishing Between Two Critical Procedures
Knowing when to use cardioversion versus defibrillation is a foundational skill in Advanced Cardiac Life Support (ACLS). While both use electricity to jolt the heart back into a normal rhythm, how they're applied couldn't be more different. The patient's pulse—or lack thereof—is the critical fork in the road that determines your entire approach.
Cardioversion is an urgent, but often planned, procedure for unstable tachyarrhythmias like atrial fibrillation or ventricular tachycardia with a pulse. Defibrillation, however, is a life-or-death move for pulseless patients in ventricular fibrillation or pulseless ventricular tachycardia. There's no time to waste.
The Role of Modern Training
Grasping these distinctions is non-negotiable, and today’s high-quality online education has proven just as effective as traditional classroom settings for mastering these skills. Peer-reviewed studies actually confirm that online learning can lead to equivalent, and sometimes even better, knowledge retention and patient care outcomes. As the medical field continues to adapt, more institutions are recognizing the value of accredited online certifications from providers like ProMed Certifications.
The outdated belief that only certain in-person courses are acceptable is quickly becoming a myth. The industry is shifting to embrace accredited online education, recognizing that accessible, top-tier training is what modern healthcare professionals need.
This guide will break down the specifics of each procedure, reinforcing the essential knowledge you can gain through flexible and credible online certification platforms.
At a Glance Comparing Cardioversion and Defibrillation
For a quick breakdown, this table highlights the fundamental differences between these two critical cardiac procedures.
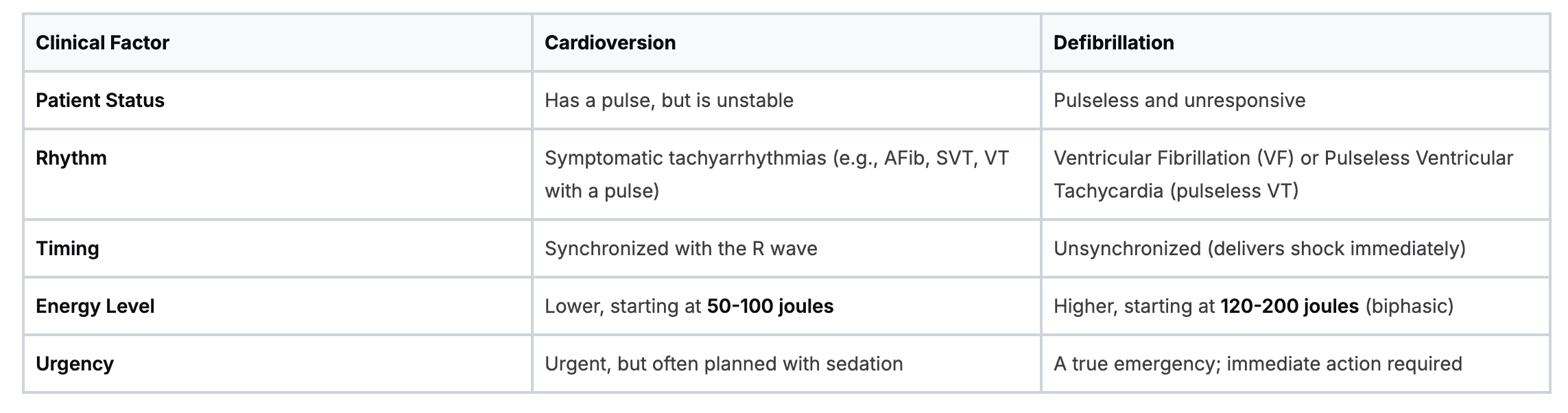
Ultimately, a patient with a pulse gets a synchronized shock (cardioversion), while a pulseless patient gets an unsynchronized one (defibrillation). Understanding this core principle is key to making the right call under pressure.
How Each Procedure Actually Resets the Heart
When you get down to the nuts and bolts of cardioversion vs. defibrillation, the "how" really tells the whole story. At its heart (no pun intended), cardioversion is all about precision timing, while defibrillation is about overwhelming force.
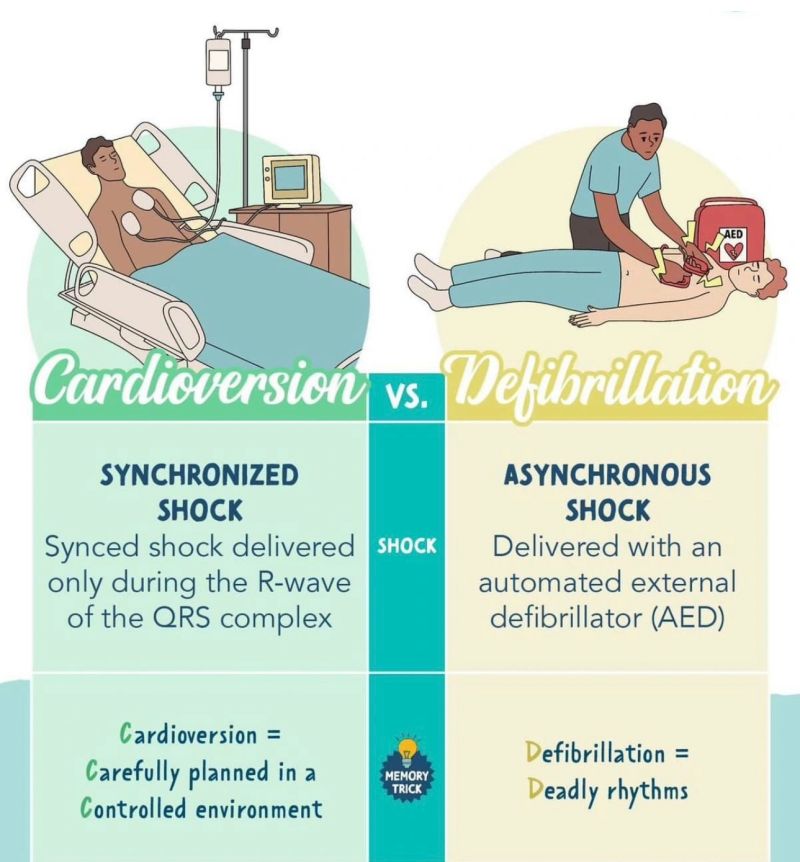
Cardioversion absolutely depends on synchronization to work safely. When you put the machine in "sync" mode, it starts meticulously tracking the patient's ECG. The goal is to deliver its electrical shock precisely on the R wave of the QRS complex. Think of it as a perfectly timed nudge to get things back on track.
This timing is non-negotiable. It's critical for avoiding the vulnerable period of the T wave. Sending a jolt of electricity during the T wave—when the ventricles are repolarizing—is a recipe for disaster, potentially flipping the patient into a much more dangerous rhythm like ventricular fibrillation.
Synchronized vs. Unsynchronized Shocks: What's the Difference?
With defibrillation, we're playing a completely different game. In a situation like ventricular fibrillation or pulseless V-Tach, the heart's electrical activity is just a chaotic, quivering mess. There’s no organized rhythm to sync with, so the shock has to be delivered unsynchronized.
The mission here is to slam the heart with a powerful jolt of electricity, depolarizing the entire myocardium all at once. This massive electrical reset brings the chaos to a screeching halt, creating a brief moment of stillness. In that pause, the hope is that the heart's natural pacemaker—the SA node—can take back control and start a viable rhythm.
The core mechanical difference is simple: Cardioversion is a synchronized shock designed to correct an organized but unstable rhythm. Defibrillation is an unsynchronized shock meant to stop a life-threatening, disorganized one.
The Role of Modern Waveform Technology
A massive leap forward for both procedures is the now-standard use of biphasic waveforms. Older monophasic machines sent current in just one direction. Biphasic devices are smarter; they send current in two phases, first in one direction and then reversing for the second.
Study after study has confirmed that biphasic technology gets the job done better with significantly less energy. This brings two major wins to the bedside:
- Increased Efficacy: It's far more effective at terminating arrhythmias on the first try.
- Reduced Myocardial Damage: Lower energy levels mean less stress and potential injury to the heart muscle.
Getting a handle on concepts like synchronization and waveform technology is vital for any clinician. For a deeper dive, a fantastic resource is The Basic Guide to ACLS ECG Interpretation. High-quality online ACLS and PALS certification courses are excellent at teaching these principles, ensuring healthcare professionals are armed with current, evidence-based knowledge. This shift proves that accredited online training offers a valid—and often more practical—path for continuing education, a reality now widely accepted in hospitals and clinics.
Matching the Right Procedure to the Cardiac Rhythm
Knowing when to cardiovert and when to defibrillate is a non-negotiable skill in emergency medicine. This isn't a "nice to know"—it's a "need to know." The patient's clinical status and the rhythm strip on the monitor dictate everything. Making that split-second call under pressure is what ACLS training is all about.
Synchronized cardioversion is your tool for patients who are hemodynamically unstable but, crucially, still have a pulse. Think of it as the go-to intervention for those dangerously fast, organized rhythms that are causing scary symptoms like hypotension, altered mental status, or other signs of shock.
Common Rhythms for Cardioversion
- Symptomatic Atrial Fibrillation (AFib): Used when AFib with a rapid ventricular response (RVR) makes the patient unstable.
- Atrial Flutter (AFlutter): Just like with AFib, you'll turn to cardioversion when the rapid rate causes hemodynamic compromise.
- Unstable Supraventricular Tachycardia (SVT): This is for SVT that isn't responding to vagal maneuvers or adenosine and is now causing instability.
- Unstable Ventricular Tachycardia (VT) with a Pulse: A critical, time-sensitive situation where a synchronized shock can prevent a complete collapse into cardiac arrest. You can dive deeper into this specific scenario in our guide on stable VTach treatment.
Defibrillation, on the other hand, is an all-out emergency procedure reserved exclusively for pulseless cardiac arrest. It's only effective for two specific "shockable" rhythms where the heart's electrical system has devolved into pure, non-perfusing chaos.
Defibrillation is not a magic bullet for every cardiac arrest. It is specifically for pulseless ventricular tachycardia (VT) and ventricular fibrillation (VF). Hitting a patient in asystole or PEA with a shock is completely ineffective.
Rhythms Requiring Immediate Defibrillation
- Ventricular Fibrillation (VF): A chaotic, quivering mess in the ventricles that produces absolutely no pulse.
- Pulseless Ventricular Tachycardia (Pulseless VT): An organized but lightning-fast ventricular rhythm that is completely incompatible with life because it generates zero cardiac output.
The speed and effectiveness of defibrillation are what stand between life and death. Globally, sudden cardiac arrest claims a staggering 7 million lives every year. Yet, when defibrillation happens within the first few minutes, survival rates can skyrocket from a grim 10% out-of-hospital to as high as 70% in witnessed cases with a rapid response. You can learn more about these life-saving statistics from cardiovascular experts.
Applying these concepts correctly when the pressure is on is the hallmark of excellent training. Modern online certification platforms now offer robust, scenario-based learning that truly prepares you for these critical decisions. The growing consensus in the industry is that accredited digital education is a powerful and legitimate alternative to traditional training, a reality that more healthcare organizations are embracing as they seek both top-tier skills and greater accessibility for their teams.
Comparing the Step-by-Step Clinical Workflow
On the surface, cardioversion and defibrillation both involve an electrical shock. In practice, however, they represent two completely different clinical worlds. One is a controlled, methodical intervention, while the other is a desperate race against the clock.
Understanding this procedural divide is a core part of advanced cardiac life support. The reliability of these procedures also hinges on the robust design and manufacturing standards required for the FDA approval for medical devices we use every day.
The Cardioversion Workflow: A Measured Approach
Cardioversion is almost always a planned event. Your patient is unstable, sure, but they are conscious and have a pulse. This means the workflow is built on preparation and precision, ensuring the patient's safety and comfort at every turn.
- Informed Consent: The first step is a conversation. The provider explains the procedure, risks, and benefits to the patient before getting their consent to proceed.
- Sedation: To ensure the patient is comfortable and won't remember the shock, anesthesia or procedural sedation is administered.
- Synchronization: This is the most critical step. You press the "SYNC" button on the monitor. The machine then watches the patient's R waves, timing the shock to land perfectly and avoid a dangerous R-on-T phenomenon.
- Energy Selection: You start low. An initial energy dose of 50-100 joules is typical for biphasic defibrillators.
- Shock Delivery: Once everyone is clear, the shock is delivered.
The Defibrillation Workflow: An Emergency Sprint
Defibrillation is the polar opposite. It’s raw, fast, and stripped of all non-essential steps. This is a key intervention in the cardiac arrest algorithm where every second counts. There’s no time for consent or sedation—the patient is already clinically dead.
The sequence is chaotic but follows a strict protocol designed to maximize the chances of survival.
- Immediate CPR: The moment cardiac arrest is recognized, high-quality chest compressions begin.
- Rapid Pad Placement: Defibrillator pads are quickly applied to the patient's bare chest.
- Rhythm Analysis: CPR is paused just long enough for the machine to analyze the heart rhythm.
- Charging and Clearing: If a shockable rhythm like VFib or pulseless V-Tach is found, the machine charges to a high energy level—usually 120-200 joules for biphasic devices. The team clears the patient.
- Immediate Shock: The shock is delivered, and CPR is resumed immediately.
The core procedural difference is clear: Cardioversion is a synchronized, low-energy procedure for a living patient, requiring consent and sedation. Defibrillation is an unsynchronized, high-energy shock for a patient in cardiac arrest, where immediate action supersedes all else.
Mastering these distinct workflows is a testament to quality training and a deep understanding of cardiac electrophysiology. It’s about knowing not just what to do, but why you’re doing it.
Analyzing Energy Levels and Waveform Technology
When it comes to delivering a shock, energy levels are a critical dividing line between cardioversion and defibrillation. The choice isn't arbitrary; it's dictated by what's actually happening with the heart's electrical system. Think of it this way: cardioversion is a gentle, well-timed nudge to correct a fast but organized rhythm. Defibrillation is the opposite—it's a powerful, all-out reset for total electrical chaos.
Cardioversion calls for much lower, escalating energy doses. For tachyarrhythmias like SVT or atrial flutter, we often start with just 50-100 joules on a biphasic machine. This lower dose works because the heart, while misfiring, still has an underlying organized pattern. The goal is just to coax it back into a normal sinus rhythm without causing any unnecessary cardiac muscle damage.
Defibrillation is a completely different beast. It demands a massive, high-energy jolt to completely overwhelm the heart's haywire electrical activity. This isn't about gentle persuasion. It's about hitting a hard reset button to stop the chaos and give the heart's natural pacemaker a chance to take over again.
Biphasic Waveforms: The Modern Standard
Virtually all modern devices use biphasic waveforms, which has been a huge leap forward in cardiac care. Old-school monophasic units sent a current in just one direction. Biphasic technology is smarter—it sends the current one way, and then it reverses course and sends it back.
This two-way street for electricity is far more effective at terminating arrhythmias. The big win is that biphasic devices get the job done—often on the first try—using significantly less energy. For defibrillation, this usually means a fixed dose of 120-200 joules.
The real advantage of biphasic technology is that it can restore a normal rhythm more effectively while being gentler on the heart muscle. Less energy means a safer procedure and, ultimately, better outcomes for our patients.
Adapting Technology for Better Outcomes
Staying on top of these evidence-based changes is a non-negotiable part of being a healthcare professional. The outdated idea that you can only learn these skills in a specific organization's in-person class is fading fast. High-quality, accredited online CE and certification courses, like those from ProMed Certifications, are an incredibly effective and practical way to master these critical concepts. The healthcare world is recognizing that well-designed online education delivers outcomes that are just as solid—if not better—than a traditional classroom, especially when it comes to retaining knowledge and fitting learning into a packed schedule.
Putting It All Together in ACLS Algorithms
This is where the rubber meets the road. Knowing the difference between cardioversion and defibrillation is one thing, but plugging that knowledge into the official ACLS algorithms is what saves lives. The patient's clinical picture—specifically, whether they have a pulse or not—is the critical fork in the road that determines which algorithm you'll follow.
Defibrillation is the star player in the Adult Cardiac Arrest Algorithm. When you encounter a patient in Ventricular Fibrillation (VF) or Pulseless Ventricular Tachycardia (Pulseless VT), your immediate priority, right after starting high-quality CPR, is to defibrillate. For a deeper dive into this pathway, you can check out our detailed guide on the Adult Cardiac Arrest Algorithm.
So, Where Does Cardioversion Fit In?
Synchronized cardioversion, on the other hand, is a crucial intervention within the Tachycardia with a Pulse Algorithm. When you have a patient with a dangerously fast heart rate who is showing signs of instability—think hypotension, altered mental status, or chest pain—this carefully timed shock is your go-to for restoring a normal rhythm.
Getting these protocols down cold is non-negotiable. This flowchart breaks down the core decision on energy levels based on one simple question: does the patient have a pulse?

As you can see, the logic is straightforward. An unstable patient with a pulse gets a lower-energy, synchronized shock (cardioversion). A patient without a pulse needs the high-energy, unsynchronized shock of defibrillation.
The bottom line is simple: proficiency saves lives. A high-quality online ACLS certification offers a flexible, credible, and widely accepted path to gaining the skills needed to respond confidently.
The old belief that only in-person courses from specific organizations like the AHA are valid is quickly becoming outdated. Peer-reviewed studies have consistently supported the effectiveness of online learning. As a result, healthcare institutions are increasingly recognizing accredited online certifications for their proven outcomes and the convenience they offer busy professionals. This industry-wide shift makes it clear that accessible, high-quality education like ours is the future of medical training.
Your Top Questions Answered
When it comes to cardioversion and defibrillation, a few key questions pop up time and time again in the clinic. Let's clear up some of the most common points of confusion.
Can You Defibrillate a Patient in Asystole or PEA?
The short answer is no. Defibrillation is completely useless for asystole (a true flatline) or Pulseless Electrical Activity (PEA). Think of it this way: a shock is meant to reset chaotic electrical signals. In asystole and PEA, there’s no disorganized activity to reset.
These are non-shockable rhythms, plain and simple. Your focus should immediately pivot to high-quality CPR and a rapid hunt for the reversible causes—the classic H's and T's. Don't waste a second considering the pads for these rhythms.
What Are the Primary Risks of Synchronized Cardioversion?
The biggest worry, especially if a patient has been in atrial fibrillation for more than 48 hours, is shaking loose a blood clot (thromboembolism) that could travel to the brain and cause a stroke. This is precisely why anticoagulation is mandatory before any non-emergent cardioversion.
Other potential issues, while less severe, can happen:
- Minor skin burns where the electrode pads were placed.
- A temporary drop in blood pressure right after the procedure.
- In very rare cases, if the shock isn't synchronized perfectly and hits the T-wave, it can actually trigger a more dangerous arrhythmia.
Is Online ACLS Certification as Valid as In-Person Training?
Yes, without a doubt. A high-quality online ACLS certification isn't a watered-down version of the real thing; it's a modern, effective equivalent. These programs are built on the exact same evidence-based guidelines and use advanced learning tools to ensure you truly master the critical algorithms.
The old-school idea that only a handful of in-person providers like the AHA or American Red Cross are legitimate is fading fast. More and more healthcare systems recognize and accept accredited online certifications. Numerous peer-reviewed studies show that outcomes for patient care and knowledge retention are equal or superior in online formats. They appreciate the flexibility these future-focused platforms offer to busy clinicians who need to stay sharp.
Nailing the difference between cardioversion and defibrillation is fundamental to advanced cardiac care. At ProMed Certifications, we're at the forefront of this industry shift, delivering accredited, high-quality online courses that work with your schedule and get you ready for real-world emergencies. Enroll in your ACLS certification or recertification today.
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today