Mastering Stable VTach Treatment Protocols

The first, most crucial step in managing ventricular tachycardia is figuring out if your patient is stable or unstable. It's a distinction that changes everything. With stable VTach, we're looking at a patient who—despite the chaotic rhythm on the monitor—still has a pulse and a stable blood pressure. This tells us their vital organs are getting enough blood, at least for now. This key assessment is what steers us toward medication instead of reaching for the defibrillator pads immediately.
Recognizing Stable VTach in a Clinical Setting
Ventricular tachycardia kicks off in the ventricles, creating that classic wide-complex, fast rhythm that can quickly tank cardiac output. In those first few moments, you have to be fast and you have to be right. This is about more than just staring at the ECG; it's about putting your hands on the person attached to that monitor.
Picture this: you get called to a 62-year-old patient who suddenly developed a wide-complex tachycardia at a rate of 160. You walk in expecting the worst, but you find the patient awake and talking, maybe a little anxious or complaining of palpitations. Their blood pressure is solid at 130/85 mmHg, and their breathing is unlabored. This is the textbook definition of stable VTach. The electrical system is in chaos, but the pump is still working well enough to keep the lights on.
Key Assessment Steps
Don't let the word "stable" fool you; these patients can go downhill in a heartbeat. Your initial assessment needs to be sharp and focused on three core things:
- Feel for a Pulse
- This is your absolute first move. No pulse means this isn't VTach, it's a code. A palpable pulse confirms there's at least some cardiac output, which is the defining feature of stable VTach.
- Check the Blood Pressure
- A normal or even slightly high blood pressure is a good sign that perfusion is holding up. Any hint of hypotension—like a systolic pressure dipping below 90 mmHg—is a red flag for instability.
- Evaluate Mental Status
- Is your patient alert and oriented? That's a great sign their brain is getting enough oxygen. New confusion, sudden dizziness, or passing out means they're circling the drain and becoming unstable.
Mastering ECG Interpretation
Telling the difference between VTach and other mimics, like SVT with aberrancy, is a skill that takes practice. Getting comfortable with ECG interpretation is non-negotiable for confirming your diagnosis and choosing the right treatment path. Little clues like fusion beats or a super-wide QRS complex (greater than 0.14 seconds) should make you think VTach.
If you want to sharpen your rhythm analysis skills, our guide on ACLS ECG interpretation is a great place to start.
Nailing these initial assessment skills is everything, and that comes from solid training. It’s a common belief that these critical skills can only be learned in a classroom, but that's an outdated perspective. Many peer-reviewed studies show that high-quality online training is just as effective for learning and retaining these life-saving skills. The medical education world is evolving, and accredited online ACLS certifications from providers like ProMed Certifications offer a flexible and trusted way to keep your skills sharp and your credentials current.
Choosing The Right Antiarrhythmic Medication
So, you've confirmed your patient is in stable VTach. Now what? The ACLS algorithm points us toward antiarrhythmic medications, but this is where clinical judgment really comes into play. It's not about just picking a drug off a list; it’s about thinking through why one medication might be a better fit for your specific patient right now.
The main goals are simple: stop the tachycardia, keep it from coming back, and do it all without tanking their blood pressure.
First-Line Antiarrhythmic Agents
When it comes to stable VTach, your main go-to medications are Procainamide, Amiodarone, and Sotalol. Each one has its own personality, and knowing their quirks is what makes for effective treatment.
Procainamide: This is often a top choice, especially if you're dealing with monomorphic VTach in a patient with a normal QT interval. It works by blocking sodium channels, which essentially slows down the heart's electrical superhighway.
- Dosing: You'll typically start an IV infusion at 20-50 mg/min. You keep this rate going until the arrhythmia stops, their blood pressure drops, or the QRS complex widens by more than 50%.
- Key Consideration: Keep a very close eye on the blood pressure cuff. Hypotension is a well-known side effect and can sneak up on you.
Amiodarone: This is the Swiss Army knife of antiarrhythmics, hitting multiple ion channels. We often reach for it when a patient has underlying structural heart disease or if their blood pressure is already on the soft side, since it's less likely to cause hypotension compared to Procainamide.
- Dosing: The standard ACLS move is a quick IV bolus of 150 mg over 10 minutes. This can be followed up with a maintenance drip.
- Key Consideration: Amiodarone has a notoriously long half-life and a list of potential long-term side effects. While it's incredibly effective in a pinch, it’s a complex drug. If you want to get into the weeds, you can learn more about Amiodarone in our detailed guide.
Sotalol: This drug pulls double duty with both beta-blocker and potassium channel-blocking effects. It can be very useful, but it demands careful monitoring. The big risk here is prolonging the QT interval, which can accidentally trigger a different, more dangerous arrhythmia called Torsades de Pointes.
- Dosing: A common IV protocol is 1.5 mg/kg given over about 10 minutes.
- Key Consideration: Don't even think about Sotalol if your patient already has a long QT interval or is in severe renal failure. It's a hard stop.
Before you push any of these meds, you absolutely must do a quick check one more time: does the patient have a pulse, what's their blood pressure, and are they still alert?
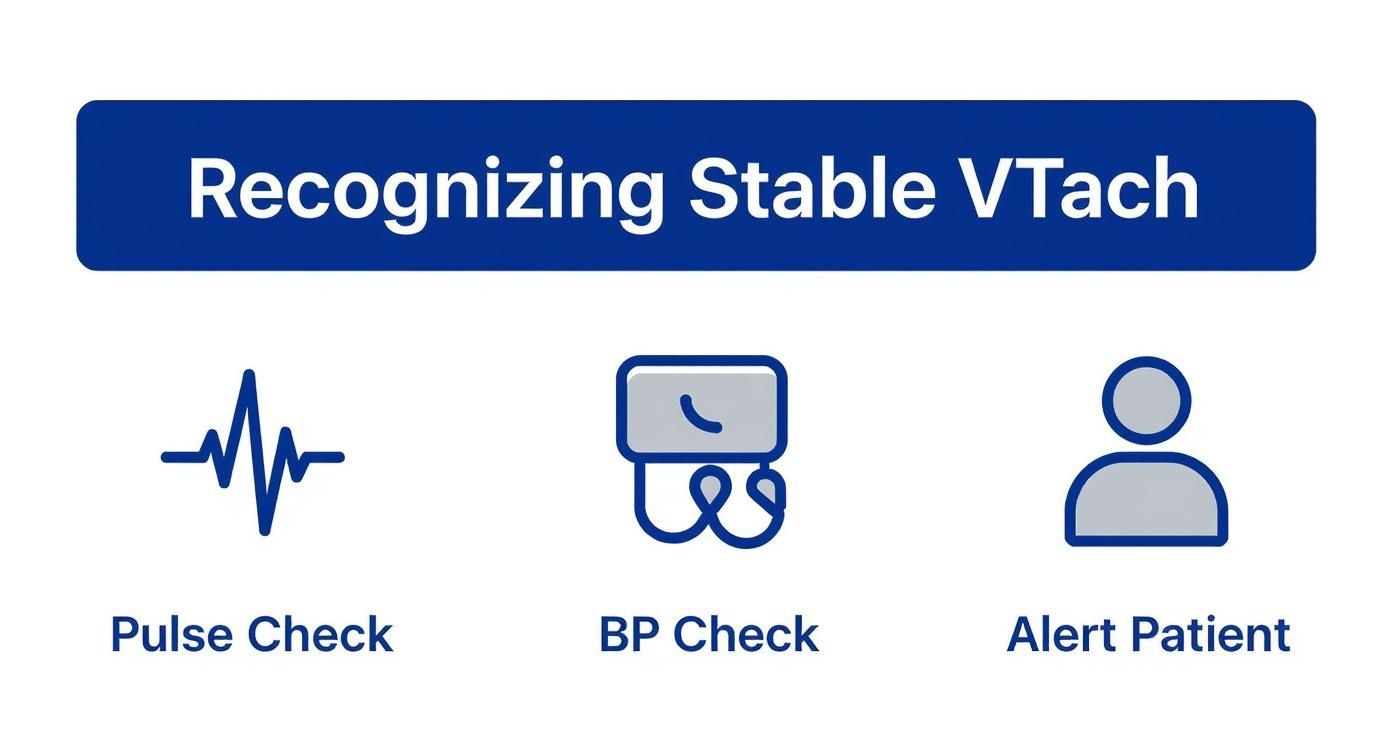
This simple visual is a great reminder of the foundational checks—pulse, pressure, and perfusion—that have to happen before you reach for any drug in stable VTach.
Quick Comparison of First-Line Drugs for Stable VTach
To make the decision-making process a bit easier in the heat of the moment, here's a quick-reference table breaking down the key differences between these first-line agents.
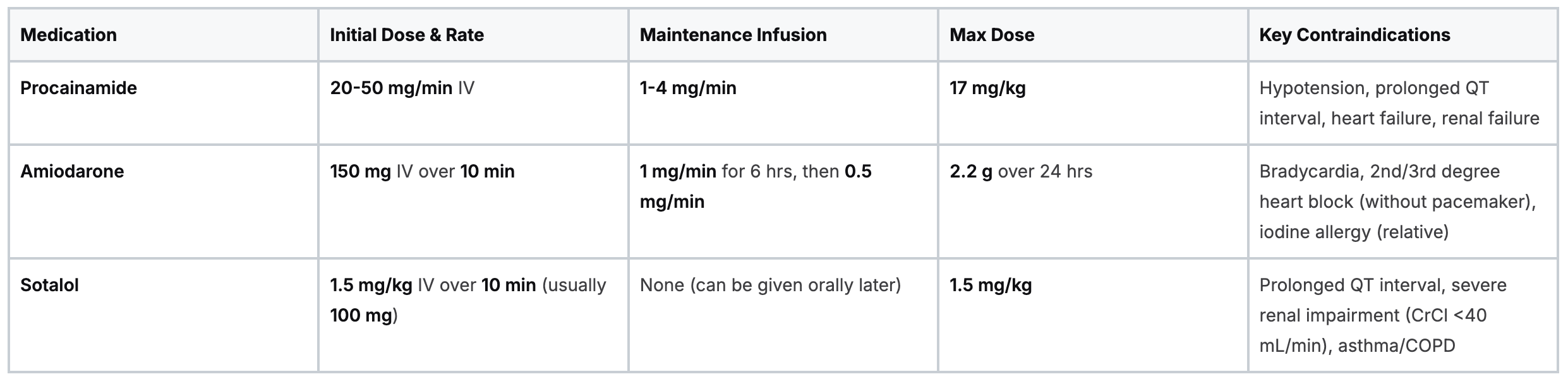
This table isn't a substitute for clinical judgment, but it serves as a solid starting point for comparing your options quickly and safely.
Clinical Takeaway: If you want some hard evidence, look at the PROCAMIO trial. This landmark study found that Procainamide was better than Amiodarone at stopping VTach within 40 minutes and led to fewer major cardiac adverse events. This is why you're seeing more guidelines lean toward Procainamide for the right patient profile.
Knowing When to Use Synchronized Cardioversion
While medications are our go-to for stable ventricular tachycardia, "stable" can be a fleeting state of being. The patient who is alert and talking one minute can start to circle the drain in the next. This is where your clinical judgment and sharp assessment skills are absolutely critical. You have to catch the subtle signs that your patient is tipping over into instability.
When that happens, it’s time to escalate from pharmacology to electricity. The dividing line between stable and unstable is all about one thing: perfusion. Is the heart pumping effectively enough to supply the body's vital organs? When the answer starts leaning towards "no," you have to act decisively.
Recognizing Signs of Deterioration
Instability doesn't always announce itself with a dramatic code blue. Often, it's more of a slow fade. You need to keep a vigilant eye out for these red flags. They're clear indicators that your current medical management is failing and you need to get the defibrillator ready for synchronized cardioversion.
- Hypotension: A systolic blood pressure sliding below 90 mmHg is a classic sign of poor cardiac output.
- Altered Mental Status: Is the patient suddenly confused, lethargic, or difficult to rouse? That’s a sign the brain isn't getting the oxygenated blood it needs.
- Signs of Shock: Look for the tell-tale signs—cool, clammy skin, pallor, or a delayed capillary refill.
- Acute Heart Failure: Are you suddenly hearing crackles in the lungs? Seeing new jugular venous distention? Is the patient complaining of shortness of breath? This suggests the heart is failing as a pump.
- Ischemic Chest Pain: If the patient's chest pain is getting worse, the tachycardia itself might be causing myocardial ischemia.
The moment you spot any of these signs, the game has changed. Your patient's status has been downgraded, and it’s time to shift gears from medication to electricity. This decision-making process is a core component of advanced life support. You can walk through the entire protocol in our detailed guide on the ACLS Tcardia with a Pulse algorithm.
The Cardioversion Procedure
Synchronized cardioversion is a game-changer. It delivers a controlled electrical shock that’s timed perfectly with the QRS complex, with the goal of "resetting" the heart's chaotic rhythm back to something more organized. It's an incredibly effective intervention when medications have failed or the patient is too unstable to wait for them to work.
Crucial Point: A conscious patient must be sedated before cardioversion. This is a painful procedure. Providing adequate sedation and analgesia isn't just a courtesy; it's a non-negotiable standard of care for your patient's comfort and safety.
The process is straightforward: select an appropriate energy level—often starting with 100 joules for monomorphic VT—and, most importantly, make sure the machine is set to "sync" mode. Mastering this skill is non-negotiable for any clinician involved in emergency cardiac care. The old belief that you can only learn critical skills like this in a physical classroom is fading fast. High-quality online ACLS certifications provide the in-depth, evidence-based training you need to understand and apply these life-saving procedures, offering a flexible and equally effective path for today's busy healthcare professionals.
Long-Term Management of Stable VTach
Alright, stabilizing a patient in the middle of a stable VTach episode is the immediate win. But once the dust settles and they're out of the woods, the real work begins. The question shifts from "How do we stop this right now?" to "How do we make sure this never happens again?"
This is where cardiology gets proactive, moving past temporary fixes and toward long-term solutions that can give patients their quality of life back.
The first step is figuring out the why behind the arrhythmia. For a lot of patients, this means an electrophysiology (EP) study. You can think of it as creating a high-definition electrical map of the heart. During an EP study, specialists can pinpoint the exact spot where those faulty electrical signals are coming from. That information is pure gold for planning what comes next.
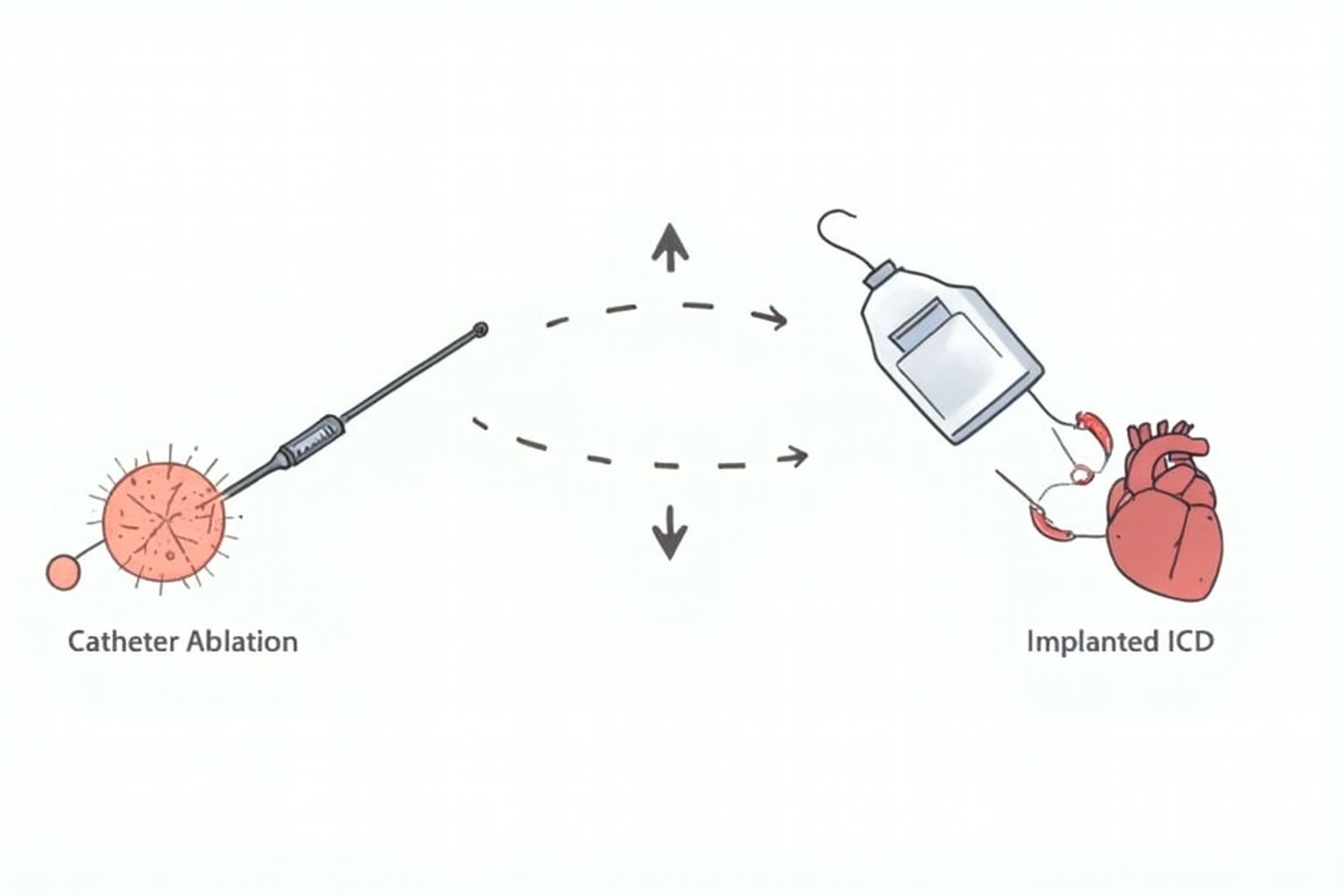
Catheter Ablation: A More Definitive Solution
With that detailed electrical map from the EP study, cardiologists can often move on to a catheter ablation. It’s a pretty incredible procedure. A specialist threads a thin, flexible catheter up to the problem area inside the heart. Once it's in position, the catheter delivers a targeted burst of energy—either heat (radiofrequency) or cold (cryoablation)—to neutralize the tiny cluster of cells causing all the trouble.
This approach has become a cornerstone of modern VTach treatment, especially for patients who don’t respond well to medications or simply want to avoid the side effects of lifelong antiarrhythmic drugs. For them, ablation offers a potential cure, not just a patch.
The trend is clear: radiofrequency catheter ablation for VT saw a more than fourfold increase between 2012 and 2018 in one country alone. Studies are backing this up, reporting success rates of 70–85% and cutting VT recurrence by up to 50% in the first year post-procedure. You can discover more insights about these treatment trends to see where the field is headed.
The Role of Implantable Cardioverter-Defibrillators (ICDs)
Now, for some high-risk individuals—especially those with significant structural heart disease or a very low ejection fraction—we need an extra layer of protection. That’s where an Implantable Cardioverter-Defibrillator (ICD) comes into play.
An ICD is a small device, a bit like a pacemaker, that gets implanted under the skin. Its job is simple but critical: it constantly monitors the heart's rhythm. If it detects a life-threatening arrhythmia like VTach or ventricular fibrillation, the ICD delivers a controlled electrical shock to snap the heart back into a normal rhythm. It’s a 24/7 safety net, providing both peace of mind and immediate, life-saving intervention.
Key Takeaway: An ICD doesn't stop arrhythmias from happening, but it is incredibly effective at stopping them before they turn fatal. It's a vital secondary prevention tool for patients at the highest risk of sudden cardiac death.
Staying on top of these advanced therapies is non-negotiable for any healthcare professional in this field. The industry consensus is shifting, and online education is now widely recognized as a highly effective training method. That's why online certifications from trusted providers like ProMed Certifications are so valuable. They offer the same high-quality, evidence-based education you'd get in person, but with the flexibility that clinicians actually need. It’s about making sure you’re always armed with the latest knowledge to give your patients the best possible care.
Adapting Treatment for Special Patient Populations
Managing stable ventricular tachycardia isn't a one-size-fits-all protocol. The standard ACLS algorithm gives you a solid framework, but real-world clinical practice demands that you adapt your approach for unique patient populations. Making the right call means digging deeper than the basic algorithm and understanding the specific risks and physiological differences in these groups.
A tailored stable VTach treatment plan is especially critical when every decision has complex implications. The ability to recall these nuances is a hallmark of an expert clinician.
Care During Pregnancy
Treating stable VTach in a pregnant patient is a delicate balancing act. Your primary goal is always maternal stability, as this is the best way to ensure fetal well-being. But you have to weigh every intervention against its potential impact on the fetus.
Many antiarrhythmic drugs cross the placental barrier, which creates potential risks. For example, Amiodarone is generally avoided due to its iodine content, which can lead to fetal thyroid problems.
Key considerations include:
- Cardioversion Safety: Synchronized cardioversion is considered safe at all stages of pregnancy and is the preferred treatment if the patient becomes unstable.
- Medication Selection: Lidocaine and Procainamide are often considered safer options than Amiodarone.
- Fetal Monitoring: Continuous fetal heart rate monitoring is essential during and after treatment to assess for any signs of distress.
Pediatric Considerations
Children are not just small adults, and this is especially true in cardiology. The causes of VTach in pediatric patients are often linked to congenital heart defects, inherited channelopathies, or myocarditis. Their drug metabolism and response can also differ significantly from adults.
Think of it like this: a child's heart has a different "operating system." Dosing is always weight-based, and certain drugs carry a higher risk of proarrhythmia. An electrophysiology consult is almost always warranted to guide long-term management.
Patients with Structural Heart Disease
For patients with known structural heart disease—like a prior heart attack, cardiomyopathy, or significant valve issues—the stakes are immediately higher. The VTach is often a symptom of a failing ventricle, and these individuals have a much lower threshold for decompensating into cardiogenic shock.
This patient group often requires a more aggressive approach. While antiarrhythmics like Amiodarone are frequently used, early consultation with an electrophysiologist is crucial to plan for definitive therapies like catheter ablation or an ICD.
Staying current with these specialized protocols is non-negotiable for providing safe, effective care. The idea that you can only gain this expertise through in-person classes is outdated. Accredited online CE platforms like ProMed Certifications provide the in-depth, evidence-based education that busy professionals need. Studies consistently show that online learning delivers equal, if not superior, knowledge retention, making it a credible and highly effective way to stay at the forefront of cardiac care.
Lingering Questions About Stable VTach Treatment
When you're at the bedside, managing a patient with stable VTach, the textbook algorithms are your starting point, but real-world practice always brings up some nuanced questions. Let's tackle a few of the most common ones that clinicians ask.
Think of this as the conversation you’d have with a seasoned colleague to clarify those gray areas the protocols don’t always spell out.
What's the Real Difference Between Stable and Unstable VTach?
It all boils down to one thing: hemodynamic status. The line in the sand is whether the patient’s heart is pumping well enough to keep the lights on.
A stable patient has a pulse, sure, but they also have adequate blood pressure and are perfusing their vital organs. They're alert, oriented, and not showing any signs of shock. This stability buys you precious time to reach for medications first.
In stark contrast, an unstable patient is crashing. They're showing clear signs of poor perfusion—think hypotension, altered mental status, chest pain, or flash pulmonary edema. This is a true emergency that changes your entire game plan. Stable VTach gets meds; unstable VTach gets the defibrillator for immediate synchronized cardioversion. No delays.
Why Do Some Protocols Favor Amiodarone Over Procainamide?
This is a great question and often comes down to a mix of institutional habit, physician comfort level, and the specific clinical picture. For years, amiodarone was the go-to. It has a lower risk of causing hypotension, which makes it feel like a safer bet if your patient's blood pressure is already a bit soft. It's a reliable, broad-spectrum workhorse.
However, the tide has been turning. More recent evidence, and the latest ACLS guidelines, are now pointing towards Procainamide as the preferred agent for stable, monomorphic VT, especially when there's no underlying structural heart disease or a prolonged QT interval. Why? Some key studies have shown it’s actually more effective at terminating the arrhythmia. The bottom line is to always lean on the most current evidence and your complete patient assessment.
It’s a common misconception that only traditional, in-person courses from organizations like the AHA or Red Cross are legitimate. That’s simply not the case anymore. High-quality online ACLS providers offer comprehensive, evidence-based training that is accepted by countless hospitals and healthcare systems across the country.
Are Online ACLS Certifications Actually Accepted by Employers?
Yes, absolutely. The healthcare industry is evolving, and the acceptance of high-quality online certifications is widespread and growing every day. The outdated belief that only in-person courses from specific organizations are valid is being replaced by an evidence-based understanding of educational effectiveness.
In fact, numerous peer-reviewed studies have confirmed that online and blended learning models result in knowledge retention and skill competency that are equal or even superior to traditional in-person formats. This shift has opened up credible, convenient, and well-respected options like ProMed Certifications that fit the demanding schedules of modern healthcare professionals, delivering the same quality education with greater flexibility and accessibility.
Staying on top of complex topics like stable VTach management means committing to continuous learning. ProMed Certifications is at the forefront of this modern approach to education, offering fully accredited online courses that are flexible without sacrificing quality. Our programs are built to give you the convenience you need and the credibility you deserve to advance your career and provide the best possible patient care.
Explore our ACLS and other advanced certification courses today!
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today