A Clinician's Guide to Post Cardiac Arrest Care

Getting a pulse back—what we call return of spontaneous circulation (ROSC)—is a huge win, but the fight is far from over. This is where post cardiac arrest care begins, and it's a critical component of saving a patient's life. Think of it as a proactive mission to shield the brain and vital organs from the damaging cascade of events that resuscitation can trigger. This guide will help you navigate the crucial steps that follow ROSC, better equipping you to improve patient outcomes.
What Happens in the First Hour After ROSC?
The moments after a patient's heart restarts are a critical turning point. This isn't the end of the emergency. It's the start of a complex, goal-directed effort to manage what's known as post-cardiac arrest syndrome. Your immediate actions here lay the groundwork for the patient’s long-term outcome, making this first hour one of the most important in their entire hospital stay.
Let's walk through the foundational ABCs of post-arrest care with a real-world scenario.
Imagine you have a 65-year-old patient who arrested in the field. You've got a pulse back. The initial chaos of CPR has calmed down, but the patient is still unconscious and unstable. Where do you even begin?
Securing The Airway And Managing Ventilation
Priority one is, and always will be, the airway. If the patient isn't awake and able to protect their own airway within 5-10 minutes of ROSC, you should plan to intubate. This isn't just about breathing; it's about taking complete control of their physiology.
Once they're on a ventilator, you can carefully manage several critical factors:
- Prevent Hypoxia: Keep their oxygen saturation between 94-98%. Dropping below this starves an already injured brain of precious oxygen.
- Avoid Hyperoxia: Just as too little oxygen is bad, too much can cause its own problems, like oxidative damage. You don't want to just blast them with 100% oxygen indefinitely.
- Maintain Normocarbia: Your target for end-tidal CO2 (ETCO2) is a normal range, typically 35-45 mmHg. This is key for regulating cerebral blood flow.
This infographic breaks down the core priorities in early post-cardiac arrest care.
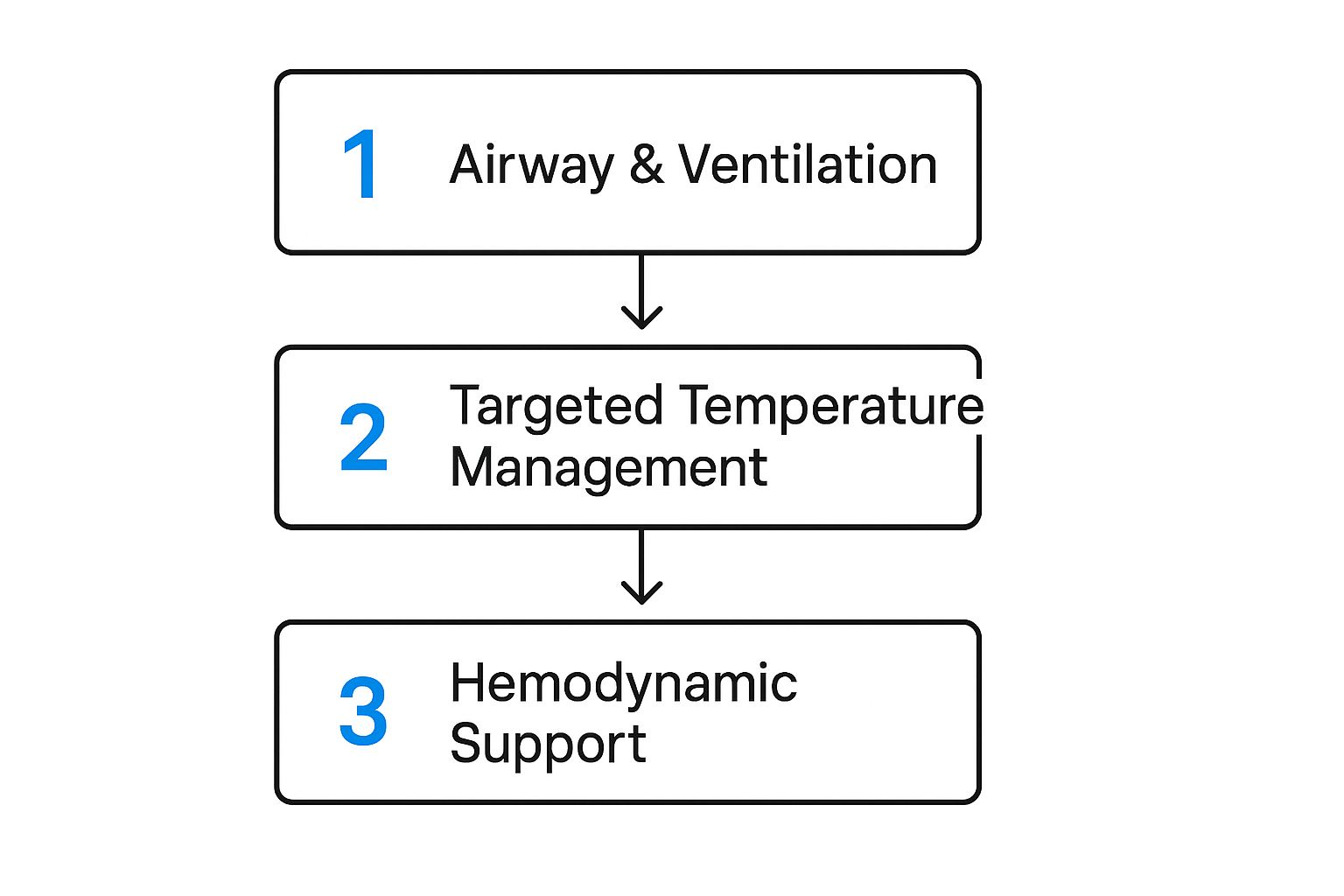
As you can see, locking down the airway and breathing is the immediate first step. This creates the stability you need to effectively manage everything else that follows, like circulation and temperature.
Stabilizing Circulation And Hemodynamics
It's common for post-ROSC patients to be hemodynamically unstable. Think of it like this: their cardiovascular system just went through a massive shock, leaving it prone to pressure failures. Your job is to restore and maintain enough pressure to perfuse the vital organs, especially the brain and heart.
A key target to aim for is a Mean Arterial Pressure (MAP) of >65 mmHg.
Getting there often requires a two-pronged approach with IV fluids and vasopressors. While the resuscitation phase of the adult cardiac arrest algorithm is behind you, its core principle of ensuring perfusion continues. A few judicious fluid boluses (say, 250-500 mL) can help with preload, but you'll often find that patients need vasopressor support, like a norepinephrine drip, to keep their pressure up without causing fluid overload.
The real challenge in post cardiac arrest care is the balancing act. You need to perfuse a post-ischemic brain that may have lost its ability to self-regulate blood flow, all while not overwhelming a stunned, post-ischemic heart.
This delicate balance requires constant monitoring and frequent reassessment. The stakes couldn't be higher. Each year, over 356,000 Americans and up to 700,000 Europeans experience an out-of-hospital cardiac arrest. With global survival rates hovering between a sobering 3-13%, optimizing every single phase of care is absolutely essential.
For a quick reference on what to prioritize in that first hour, this table breaks down the immediate goals.
Immediate Post-ROSC Stabilization Targets
These targets provide a clear, actionable roadmap for the initial phase of care.
By focusing on these foundational steps—airway, ventilation, and circulation—you build a stable platform. From here, all subsequent interventions, like targeted temperature management and detailed neurologic care, can be launched successfully. This proactive, goal-directed approach in the first hour is what gives your patient the best possible shot at a meaningful recovery.
How to Master Hemodynamic Support
Once the initial chaos settles and you've secured the airway, your focus has to pivot to the patient's hemodynamic status. This isn't just about chasing numbers on a monitor; it’s about making sure life-sustaining blood flow is reaching every organ, especially the brain and heart.
Good hemodynamic support is a cornerstone of post-cardiac arrest care. It's what prevents further injury to a system that's already been pushed to its absolute limit.

Think of the circulatory system like a complex plumbing network. After a total shutdown (the arrest), just turning the water back on isn't good enough. You have to carefully restore the right amount of pressure—not too low, not too high—to get water to every faucet without blowing out the pipes. That's exactly what we’re doing here.
The Non-Negotiable MAP Target
The most critical number you'll be watching is the Mean Arterial Pressure (MAP). The goal here is simple but crucial: consistently maintain a MAP of >65 mmHg.
Letting the pressure drop below this threshold is like a brownout for the body's organs. The ones at the end of the line, like the brain and kidneys, get starved of blood flow. This hypotension can trigger devastating secondary organ injury, undoing all the hard work you put into the initial resuscitation.
You'll almost always start with IV fluid boluses to help restore volume. But don't be surprised when that's not enough; many post-arrest patients will need more than just fluids to hit and maintain that target MAP.
Choosing and Titrating Vasopressors
When fluids alone aren't cutting it, vasopressors become your go-to tool. These medications work by constricting blood vessels, which effectively dials up the pressure inside the system.
Norepinephrine is the first-line vasopressor for most post-cardiac arrest patients. It gives you reliable vasoconstriction without cranking up the heart rate too much, which is a huge advantage when you're dealing with a stunned myocardium.
The real art of hemodynamic support is in the titration. This isn't a "set it and forget it" situation. It's a constant process of adjusting the infusion rate based on the patient's real-time response, always aiming to use the lowest effective dose to keep that MAP above 65 mmHg.
Sometimes, pressure isn't the only problem. The heart muscle itself might be too weak to pump effectively—a state we call cardiogenic shock. In these cases, you might need to add an inotrope like dobutamine to help improve the heart's contractility. The choice between vasopressors (for pressure) and inotropes (for the pump) comes down to what you're seeing in the patient in front of you.
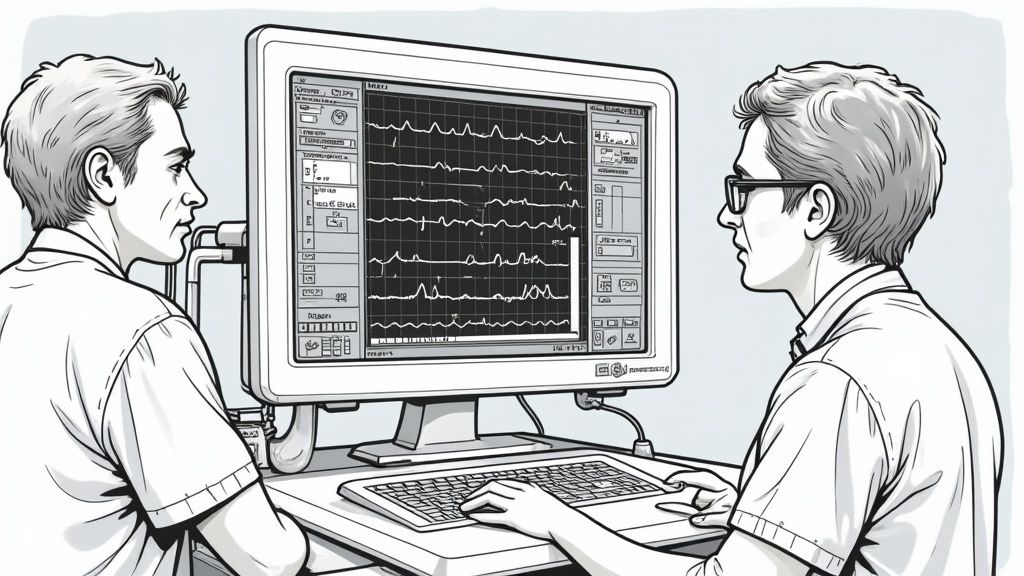
The Role of Continuous Cardiac Monitoring
While you're busy managing pressure, you also have to play detective and figure out what caused the arrest in the first place. Get a 12-lead ECG as soon as possible after ROSC. You're hunting for any evidence of an ST-elevation myocardial infarction (STEMI), which is a ticket straight to the cardiac cath lab.
Beyond that initial 12-lead, continuous cardiac monitoring is non-negotiable. It lets you keep a close eye on a few critical things:
- Arrhythmias: The post-arrest heart is incredibly irritable and can easily slip back into dangerous rhythms.
- Ischemic Changes: You might see developing signs of ischemia that weren't there on the first ECG.
- Response to Treatment: This is how you see if your vasopressors, fluids, and other interventions are actually helping the heart rate and rhythm.
A deep understanding of cardiac function is vital here, and it’s a field that's always advancing. For those interested in where cardiology is headed, resources on Innovative Heart Segmentation: AI-Driven Cardiac Insights offer a fascinating look into new technologies.
Ultimately, stabilizing hemodynamics is all about protecting the patient from that second wave of injury that comes after a cardiac arrest. By vigilantly maintaining perfusion, treating the underlying cardiac cause, and making smart medication choices, you create the stable physiological foundation needed for recovery. This meticulous management is what turns a successful resuscitation into a patient's second chance at life.
How to Implement Targeted Temperature Management
Targeted Temperature Management, or TTM, is one of the most powerful tools in our arsenal for neuroprotection after a cardiac arrest. Why does it matter to you? Because it's a true cornerstone of modern post-cardiac arrest care that directly impacts patient survival and neurological function. The basic idea is simple: we put the brain into a protected, low-energy state to give it a chance to heal.
Think of it like putting a high-performance engine on a cooling system to prevent it from overheating after being pushed to its limits. This guide will help you understand TTM so you can confidently use this life-saving technique.

Why Temperature Control Matters
After the brain is starved of oxygen during an arrest, a nasty cascade of secondary injuries kicks off the moment circulation returns. Fever is a particularly dangerous and common complication in this period, as it ramps up the brain's metabolic demand and makes neuronal damage even worse.
The goal of TTM is straightforward: prevent fever and hold the body at a constant, controlled temperature. This simple act slows down the brain’s metabolism, cuts down on inflammation, and ultimately helps preserve neurologic function.
While older protocols used to aim for deep hypothermia, the latest guidelines recommend maintaining a target temperature between 32°C and 36°C (89.6°F to 96.8°F) for at least 24 hours in any patient who remains comatose after ROSC. You can dive deeper into these protocols in our guide to the ACLS post-cardiac arrest care algorithm.
The bottom line is that actively preventing fever is non-negotiable. It's a fundamental intervention with a massive impact on your patient's outcome.
The Three Phases of TTM
Rolling out TTM successfully means guiding your patient through three distinct phases. Each one requires sharp monitoring and management to make sure they get the full neuroprotective benefit.
- Induction: This is the cool-down. Your mission here is to get the patient’s core body temperature into the target range as quickly and safely as you can. You can use anything from simple ice packs and cooling blankets to more advanced endovascular cooling catheters.
- Maintenance: Once you've hit your target temperature, the real work begins. The goal is to stay there for at least 24 hours. This requires constant core temperature monitoring—think an esophageal probe or bladder catheter—and frequent tweaks to your cooling device.
- Rewarming: After the maintenance window, the patient needs to be rewarmed slowly and carefully. A rapid temperature spike can trigger hemodynamic instability and nasty electrolyte shifts. The standard of care is a gentle rewarming of about 0.25°C per hour.
Managing Common Challenges
Of course, TTM isn't always a smooth ride. Your patient’s body is going to fight the cooling process, which leads to some predictable physiological responses you need to be ready for.
Shivering is public enemy number one. It’s the body's natural attempt to generate heat, and it can crank up metabolic demand so much that it completely negates the benefits of cooling. Getting this under control almost always requires good sedation and analgesia.
Beyond shivering, keep an eye out for these other potential bumps in the road:
- Electrolyte Imbalances: Cooling can make potassium, magnesium, and phosphate levels go haywire. Regular lab draws are a must to stay on top of these shifts.
- Bradycardia: A slower heart rate is an expected response to cooling. It's usually well-tolerated as long as the patient's blood pressure holds steady.
- Coagulopathy: Hypothermia can interfere with platelet function and the clotting cascade, which slightly bumps up the risk of bleeding.
Despite these hurdles, the neuroprotective benefits are undeniable. Cardiac arrest claims over 436,000 lives annually in the U.S. With roughly 73.4% of these events occurring at home and only about 40% of victims getting bystander CPR, every single intervention that improves outcomes is absolutely critical.
By understanding the phases of TTM and proactively managing its side effects, you can give your patients their best shot at a meaningful neurological recovery.
How to Protect the Brain with Neurologic Care
Let's be honest, the ultimate win in post-cardiac arrest care isn't just getting a pulse back. It's returning a patient to their life with their neurologic function intact. This entire section is dedicated to the most important organ of all: the brain. Shielding it from further injury after an arrest demands a deliberate, multi-pronged strategy that goes way beyond just chasing a blood pressure goal. This guide will help you understand that strategy.
We'll get into the core strategies for neuroprotection, starting with tight glucose control and seizure prevention, then move on to building an accurate neurologic prognosis.
Core Strategies for Neuroprotection
After a cardiac arrest, the brain is incredibly vulnerable. Just a few key interventions can make a world of difference in shielding it from further damage during this critical recovery window. Think of these as the fundamental guardrails you put in place to create the best possible healing environment.
- Glucose Control: One of the simplest yet most effective measures is getting blood sugar under control. Hyperglycemia is an almost universal stress response after an arrest, but we know that high glucose levels are directly linked to poor neurological outcomes. You should aim for a blood glucose between 7.8-10 mmol/L.
- Seizure Management: Another huge focus has to be on preventing and treating seizures. An injured brain is an irritable brain. Seizures dramatically crank up its metabolic demand, which only pours fuel on the fire of the initial injury. We see seizures in about one-third of post-arrest patients, making this a common and dangerous threat we must anticipate.
The Threat of Non-Convulsive Seizures
When you hear "seizure," you probably picture convulsions. The reality in the ICU is that many post-arrest seizures are non-convulsive, meaning they have no obvious physical signs. These silent seizures are just as damaging but are impossible to spot without the right tools.
This is where continuous EEG (electroencephalogram) monitoring becomes absolutely essential. Think of it like this: an EEG lets you see the brain's electrical activity, revealing seizure activity that a physical exam would completely miss. It’s the only reliable way to catch and treat non-convulsive status epilepticus.
If a comatose post-arrest patient isn't waking up as you'd expect, non-convulsive seizures need to be high on your list of suspects. Getting them on a continuous EEG is the only way to get a definitive answer and guide your treatment.
The Multimodal Approach to Neurologic Prognostication
One of the most challenging aspects of post-cardiac arrest care is figuring out a patient's long-term neurologic prognosis. Families will look to you for answers, and making a premature or inaccurate call can be devastating. The most important rule here is to never rely on a single data point.
Instead, a multimodal approach is the standard of care. This means pulling together information from multiple sources to build a comprehensive picture. Critically, this process shouldn't even begin until at least 72 hours have passed since the completion of TTM. This gives sedatives time to clear and allows the brain's initial stunning to subside.
A robust multimodal assessment has several key components:
- Clinical Examination: This is your foundation. Pay extremely close attention to pupillary and corneal reflexes. Absent pupillary light reflexes at the 72-hour mark are a very strong predictor of a poor outcome.
- Biomarkers: Certain blood tests can give you valuable clues. Neuron-Specific Enolase (NSE) is a protein dumped into the bloodstream by damaged neurons. Persistently high levels can point toward severe brain injury.
- EEG Patterns: Beyond just sniffing out seizures, the background EEG pattern itself is incredibly telling. A suppressed or burst-suppression pattern often suggests a very poor prognosis.
- Imaging Studies: A head CT is great for ruling out catastrophic events like a massive stroke or hemorrhage. An MRI can give you a much more detailed map of the extent of the hypoxic-ischemic brain injury.
By pulling all this information together, you can move from a place of uncertainty to a well-supported, evidence-based prognosis. This is what allows you to have compassionate, realistic conversations with families, guiding them through unimaginably difficult decisions with clarity and confidence. It’s this thoughtful, systematic approach that truly defines excellent neurologic care after cardiac arrest.
How It Works in the ICU: Holistic Management
Getting a pulse back is just the first battle. The real war is won in the ICU, where we tie everything together—hemodynamics, temperature control, and neurologic protection—into a cohesive, patient-centered plan. This is where we shift from reactive, life-saving maneuvers to a proactive strategy for long-term recovery.
It’s about looking at the patient as a whole. Every detail, from ventilator settings and sedation to nutrition and diagnostics, has to be dialed in perfectly. Our focus moves from the immediate crisis at the bedside to paving a clear road to recovery.
Lung-Protective Ventilator Strategies
Once a patient is intubated, the ventilator becomes one of our most powerful—and potentially dangerous—tools. The absolute goal is a lung-protective strategy to prevent ventilator-associated lung injury (VALI), a nasty complication we see all too often in critically ill patients.
The core of this approach is using low tidal volumes, typically 6-8 mL per kilogram of ideal body weight. Think of it like inflating a delicate balloon. You want to use just enough air to expand it without causing overstretching and damage. This simple step goes a long way in reducing lung strain and inflammation.
Of course, we also need to use the right amount of Positive End-Expiratory Pressure (PEEP). PEEP helps keep the tiny air sacs (alveoli) open, which is critical for good oxygenation. It's a constant balancing act—enough PEEP to support the lungs, but not so much that we tank the patient's blood pressure.
Navigating Sedation and Nutrition
Sedation is a double-edged sword in post-arrest care. It's essential for managing discomfort and stopping shivering, but if we go too deep or too long, we can completely mask the underlying neurologic exam.
The best practice here is to stick with short-acting agents like propofol or remifentanil. This lets us perform daily "sedation vacations," where we pause the meds to get a clean window for a reliable neuro assessment. It's all about balancing patient comfort with our need for clear diagnostic information.
And don't forget nutrition. Post-arrest patients are in a hypermetabolic state, burning through energy reserves like crazy. Starting enteral nutrition (tube feeding) within 24-48 hours is crucial. It provides the fuel the body desperately needs to heal.
Pinpointing the Root Cause
While we're busy managing the fallout from the arrest, we also have to put on our detective hats and figure out what caused it in the first place. A patient’s recovery often hinges on finding and treating the original problem.
Our diagnostic journey needs to be systematic and thorough:
- Cardiac Causes: A 12-lead ECG and an echo are non-negotiable first steps. If you see a STEMI, the patient needs to get to the cath lab, period.
- Pulmonary Causes: A chest X-ray or CT scan can quickly spot things like a massive pulmonary embolism, pneumonia, or a pneumothorax.
- Toxicological Causes: If there's any suspicion of an overdose, a comprehensive toxicology screen is a must. You might find a specific antidote that could turn things around.
- Neurologic Causes: A head CT is vital to rule out a catastrophic intracranial event, like a hemorrhage, that could have triggered the arrest.
This detective work is so critical because out-of-hospital cardiac arrest (OHCA) remains a huge public health challenge. Data shows that in 2015, there were around 347,000 EMS-assessed OHCAs in the United States, with a staggering 73.9% happening at home. With nearly half of all arrests being unwitnessed, getting to the root cause is a fundamental part of providing effective care.
Planning for the Road to Recovery
Great ICU care always looks beyond the immediate crisis. From day one, we should be thinking about the next steps. This means having ventilator weaning protocols ready, getting physical and occupational therapists involved early, and, most importantly, keeping the family in the loop.
Keeping families informed and involved isn't just a courtesy; it's a core component of patient-centered care. They provide invaluable history, act as advocates, and are essential partners in the long and often difficult decision-making process.
As patients stabilize, it's our job to help families understand the long-term journey ahead. For those whose arrest was cardiac in nature, explaining a typical heart attack recovery timeline can give them a helpful roadmap and manage expectations. This kind of forward-thinking approach creates a smoother transition from critical care to rehab and gives our patients the best possible shot at a meaningful recovery.
Common Questions in Post-Arrest Care
When you're managing a patient after cardiac arrest, things move fast. It's a high-stakes environment where the decisions you make in the first few hours can dramatically impact outcomes. Let's walk through some of the most frequent questions that come up in the trenches of post-arrest care.
What Is The Top Priority Immediately After ROSC?
The second you get a pulse back, you're fighting a new battle on two fronts: preventing the patient from re-arresting and protecting their brain from secondary injury. You have to tackle both at once.
Your immediate focus should be on aggressive hemodynamic stabilization. Get that blood pressure up and keep it there. The goal is a Mean Arterial Pressure (MAP) of >65 mmHg. At the same time, you need to manage their breathing and oxygen levels carefully. We're aiming for an SpO2 of 94-98% — enough to perfuse the brain, but not so much that we cause hyperoxic damage. A rapid 12-lead ECG is another non-negotiable step to hunt for a STEMI.
When Should We Start Targeted Temperature Management?
The short answer? As soon as possible.
For any comatose adult who has achieved ROSC, Targeted Temperature Management (TTM) needs to be on your immediate to-do list, no matter what their initial rhythm was. The neuroprotective clock is ticking, and the benefits of cooling are incredibly time-sensitive. Don't wait until the patient is settled in the ICU; this process should start right there in the Emergency Department.
The goal is to reach your target temperature quickly and hold it for at least 24 hours. This gives the brain the best possible environment to begin healing and reduces the risk of devastating secondary injury.
How Do You Accurately Determine Neurological Prognosis?
This is a tough one, and it's where patience becomes a virtue. You should never make a call on neurological prognosis based on a single finding or a quick exam in the first day or two. It's a recipe for getting it wrong.
A reliable prognosis requires a multimodal approach, and it shouldn't even be attempted until at least 72 hours after the patient has been rewarmed from TTM. This crucial waiting period allows sedatives to wash out and gives the brain time to recover from the initial shock of the arrest.
A solid assessment pulls together information from several sources:
- The Clinical Exam: Are pupillary and corneal reflexes present? This is a cornerstone of your evaluation.
- Biomarkers: A blood test for Neuron-Specific Enolase (NSE) can give you a clue about the extent of neuronal damage.
- Continuous EEG Data: This is vital for spotting non-convulsive seizures and assessing the brain's background activity.
- Advanced Neuroimaging: An MRI can paint a very clear picture of any hypoxic-ischemic injury.
Piecing all of this data together is how you build a comprehensive and reliable prognosis, which is absolutely essential for guiding treatment and having honest conversations with the family. Mastering these post-arrest concepts is a key part of advanced resuscitation.
This guide should lay the framework for a systematic and effective approach to post-arrest care. By mastering these concepts, you can confidently navigate the complexities of this critical phase and give your patients the best possible chance at a meaningful recovery. Completing an ACLS certification can help cement this knowledge.
At ProMed Certifications, we are committed to providing high-quality, accessible medical education that empowers healthcare professionals to deliver the best possible patient care. To advance your skills in post-arrest management and other critical areas, explore our full range of certification courses at https://promedcert.com.
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today