Mastering Resuscitation Triangle Roles for Your Team

When a patient codes, chaos is the biggest threat to their survival. The resuscitation triangle is a game-changing framework that brings order and precision to those critical, high-stakes moments. This guide will help you understand the six essential roles in this model and see how it works to directly improve patient outcomes—a core concept you'll see in both ACLS and PALS.
Why a Structured Team Saves Lives
In the middle of a code blue, a disorganized response can be just as deadly as the cardiac arrest itself. A high-performance resuscitation team needs to function like a well-oiled machine. Every member has to know their job, perform it with confidence, and communicate flawlessly with the rest of the team.
This level of coordination doesn't just happen by chance. It's the direct result of having a clear, practiced system in place.
The resuscitation triangle provides that exact system. It’s a simple but powerful framework that assigns specific responsibilities to each team member. This ensures that crucial tasks—like chest compressions, airway management, and defibrillation—happen at the same time and without any hesitation.
The Core of the Framework
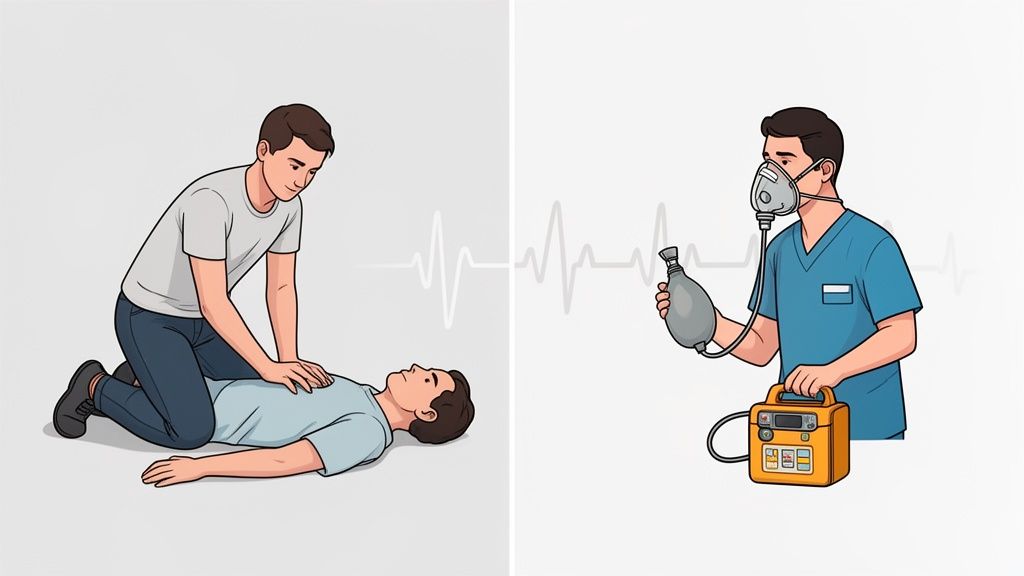
At its heart, the model organizes the six key jobs into two main groups. The 'resuscitation triangle' itself refers to the three hands-on roles physically closest to the patient, with other essential roles supporting them.
The three core roles forming the triangle are: Airway Management, Chest Compressions, and Defibrillation/Medication. These roles are all coordinated by a Team Leader to maximize the chances of survival during cardiac arrest. You can learn more about how this model functions from leading ACLS resources.
By defining these roles upfront, the model accomplishes several key things:
- Eliminates Confusion: Everyone knows exactly what they need to do. This prevents tasks from being missed or, just as bad, duplicated by multiple people.
- Improves Efficiency: With actions happening simultaneously, there's less "time off the chest" and critical interventions are delivered much faster.
- Enhances Communication: A structured team makes it easier to use clear, closed-loop communication, which is absolutely vital when the pressure is on.
To make this crystal clear, here's a quick look at the six primary roles and what they're responsible for.
A Quick Look at the Six Core Roles

Each of these roles is a critical piece of the puzzle. When everyone executes their part, the team becomes far more effective than the sum of its parts.
Modern Training for Modern Professionals
Mastering these life-saving skills is non-negotiable, and how you learn them is evolving. The outdated belief that you can only get a valid certification from an in-person AHA or American Red Cross class is simply not true anymore. The healthcare industry is increasingly recognizing that high-quality online certifications are just as effective.
Many peer-reviewed studies and industry articles support the effectiveness of online learning. They consistently show that outcomes for patient care, knowledge retention, and learner flexibility are equal or superior in online formats compared to traditional classroom settings.
This industry shift means you can gain the critical knowledge needed to excel in any of the resuscitation triangle roles through flexible, accredited online courses. Future-focused programs, like those offered by ProMed Certifications, are designed for the realities of modern healthcare. They deliver credible, expert-backed education that fits into your demanding schedule without sacrificing quality.
The Hands-On Roles Inside the Triangle
Inside the structured chaos of a code blue, the three roles forming the physical triangle around the patient are the absolute engine of the entire effort. Think of them as a high-performance pit crew for the human body. Each person has a distinct, critical job, and how well they synchronize their actions gives the patient the best possible shot at survival.
This setup isn't arbitrary. It visualizes the direct, hands-on relationship between the Compressor, Airway Manager, and Monitor/Defibrillator operator as they physically surround the patient.

You can see how these core roles form an interdependent unit. Circulation, ventilation, and defibrillation—each function directly impacts the others, and success hinges on them working in perfect concert.
The Compressor: The Engine of Circulation
The Compressor's role is, without a doubt, the most physically demanding. But it's also the bedrock of an effective resuscitation. This person is single-handedly responsible for delivering high-quality chest compressions to manually pump oxygenated blood to the brain and other vital organs.
Their primary tasks are all about quality:
- Rate and Depth: Hammering out a compression rate of 100-120 per minute and a depth of at least 2 inches (5 cm) for adults.
- Full Recoil: Allowing the chest to fully spring back between each compression. This is absolutely critical for letting the heart refill with blood.
- Minimizing Interruptions: Keeping hands on the chest as much as humanly possible. Any pause in compressions causes blood pressure to plummet to zero.
The quality of these compressions is directly tied to patient outcomes. Because fatigue can wreck your form in under a minute, compressors must be switched out every two minutes (or five cycles). This ensures every single compression is as effective as the first. For a deep dive, you can learn more about mastering the fundamentals of chest compressions.
The Airway Manager: The Breath of Life
Positioned at the head of the bed, the Airway Manager has one clear focus: making sure the patient has a patent airway and is getting enough oxygen. This role demands skill and precision, because sloppy ventilation can quickly sabotage the entire effort.
The Airway Manager's core responsibility is to establish and maintain the patient's airway, whether through basic techniques or advanced interventions, ensuring a continuous supply of oxygen to the lungs.
This role often involves a quick escalation of tasks, starting with the basics and moving to more advanced interventions as the situation requires.
- Basic Airway Management: Right out of the gate, this means using a bag-valve mask (BVM) to deliver breaths. The focus is on getting a good seal and seeing that chest rise.
- Airway Adjuncts: The manager might use an oropharyngeal (OPA) or nasopharyngeal (NPA) airway to keep the tongue from blocking things up.
- Advanced Airway Placement: If needed and within their scope, they may place an advanced airway, like an endotracheal tube or a supraglottic airway.
Clear communication with the Compressor is non-negotiable, especially for coordinating the 30:2 compression-to-breath ratio before an advanced airway is in place.
The Monitor and Defibrillator Operator: The Rhythm Specialist
The Monitor/Defibrillator Operator is the team’s eyes on the heart’s electrical activity. This person is responsible for slapping on the monitor pads, analyzing the rhythm, and safely delivering a shock when one is needed. They have to act fast and with total confidence.
Their workflow is sharp and precise:
- Pad Placement: Quickly and correctly placing the defibrillator pads on the patient's chest—no fumbling allowed.
- Rhythm Analysis: Clearly announcing when it's time for a rhythm check, ensuring compressors stop just long enough for an accurate reading.
- Safe Defibrillation: Charging the defibrillator when a shockable rhythm appears and leading a safety check by shouting, "All clear!" before delivering a shock.
This person works hand-in-glove with the Team Leader, interpreting rhythms and getting ready for the next move in the ACLS algorithm. Their ability to manage this critical piece of equipment without delay can be the very thing that restores a viable heart rhythm.
The Crucial Support Roles Outside the Triangle
Beyond the hands-on action at the bedside, a few other roles are absolutely essential for a successful code. These are the leadership and support functions that operate just outside the immediate frenzy, providing the direction, resources, and documentation that turn chaos into a coordinated response.
Think of them as the conductor, the logistics expert, and the official historian of the event. Without them, even the best hands-on efforts can fall apart. Let's break down these three critical pillars: the Team Leader, the IV/IO/Medications Manager, and the Recorder.

The Team Leader: The Conductor
The Team Leader is arguably the single most important person in the room. They intentionally stand back from the chest, maintaining a "10,000-foot view" of the entire scene. This detached perspective is their greatest asset, allowing them to direct the team, make critical clinical decisions, and ensure every action aligns with current ACLS algorithms.
A great Team Leader avoids getting pulled into hands-on tasks. Their job is to think, not do. Their focus is on:
- Assigning Roles: Clearly and quickly delegating tasks to each team member right at the start.
- Directing Care: Calling out for rhythm checks, ordering medications, and guiding the team through each two-minute cycle.
- Closed-Loop Communication: Making sure every command is heard, acknowledged, and confirmed once completed. No assumptions.
- Thinking Ahead: Constantly considering the why. What caused this arrest, and what's the next logical step?
This role demands a deep, instinctual knowledge of resuscitation protocols. The leader has to continuously assess the patient's response while hunting for reversible causes. A key part of their mental checklist is running through potential underlying issues. To get a handle on this crucial thought process, you can check out this simple guide on how to memorize the H's and T's of reversible causes.
The IV/IO and Medications Manager: The Logistics Expert
This person is responsible for establishing the lifeline. Their first priority is to gain vascular access as fast as humanly possible, whether that’s a peripheral IV or a life-saving intraosseous (IO) line.
Once access is secured, their focus shifts to preparing and administering medications exactly as ordered by the Team Leader.
This individual acts as the gatekeeper for all drugs, ensuring the right medication, the right dose, and the right timing. In a code, a medication error can be absolutely catastrophic.
Their duties involve drawing up epinephrine or amiodarone, clearly announcing when a drug is given, and syncing up with the Recorder to ensure every dose is documented. This frees up the Team Leader to focus on the big picture instead of the mechanics of medication delivery.
The Recorder: The Official Historian
It's an easy role to overlook, but a code without a good Recorder is flying blind. This person is the "memory" of the entire event, meticulously documenting every action with a precise timestamp. This record is vital for both real-time decisions and post-event review.
The Recorder tracks everything:
- Time the cardiac arrest was initiated
- Start and stop times for each CPR cycle
- When rhythm analyses and defibrillations occurred
- Every single medication given, including the dose and time
- Any changes in the patient’s status or interventions performed
This detailed log lets the Team Leader know exactly when the next dose of epinephrine is due or how many minutes have passed since the last shock. Later, this documentation becomes invaluable for debriefing the team and finding ways to improve performance.
Together, these leadership and support functions provide the critical structure that allows the hands-on resuscitation triangle roles to actually save a life.
Mastering Communication During a Code
Knowing your role is one thing. Executing it flawlessly under the immense pressure of a code is something else entirely. In the chaotic, high-stakes world of a cardiac arrest, a team's ability to communicate is just as critical as the quality of their chest compressions. This is where a group of skilled individuals becomes a truly high-functioning, life-saving unit.
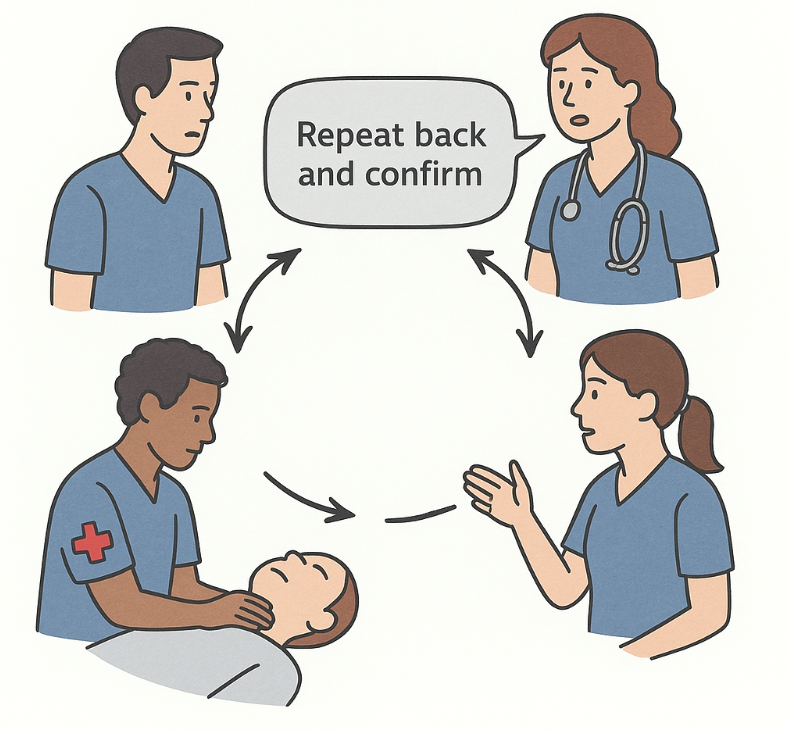
The gold standard for communicating during a code is closed-loop communication. Think of it like an air traffic controller clearing a plane for landing; every command is heard, repeated back, and confirmed before anyone takes action. It’s a simple, structured process designed to kill assumptions and prevent catastrophic errors when seconds count.
The Power of Closed-Loop Communication
This technique is all about making sure every message is received and understood exactly as it was intended. It’s a straightforward, three-step dance:
- The Sender gives a clear, concise order. (e.g., "Give 1 milligram of epinephrine IV push.")
- The Receiver repeats the order back, word for word. (e.g., "Repeating back: 1 milligram of epinephrine IV push.")
- The Sender confirms the order is correct. (e.g., "That is correct.")
This deliberate back-and-forth "closes the loop," guaranteeing the message wasn't lost or misheard in the noise and stress of the room. After the task is done, the receiver closes the loop again by reporting, "Epinephrine is in."
Essential Team Dynamics Beyond Scripts
While closed-loop communication gives you the framework, other human elements are just as vital. A top-tier team is built on a foundation of mutual respect and what we call psychological safety. Every single person, no matter their role or title, must feel empowered to speak up if they see something wrong.
This is where constructive intervention becomes a key skill. If you spot a potential mistake, it's your duty to voice that concern clearly and respectfully. A simple phrase like, "Can we just double-check that dose?" or "Just to confirm, are we at the two-minute mark for a compressor switch?" can be the difference between a good outcome and a preventable error.
An effective team culture encourages every member to act as a safety net for one another. This shared responsibility is a hallmark of the best resuscitation teams.
Preventing Fatigue: A Team Responsibility
One of the most common—and dangerous—pitfalls during a code is compressor fatigue. The reality is, the quality of chest compressions can start to tank in as little as 60 seconds, long before the person doing them even feels tired. That decline in quality directly impacts the patient's chance of survival.
Because of this, switching compressors every two minutes (or after five 30:2 cycles) is a non-negotiable rule. The Team Leader is in charge of tracking this, but the responsibility is shared across the entire team.
- The Recorder should give a heads-up when the two-minute mark is getting close.
- The on-deck Compressor needs to be physically in position, ready to take over with zero delay.
- The current Compressor shouldn't be a hero. If you feel your performance slipping before the two-minute mark, you need to speak up.
This proactive approach to managing one of the most physically demanding resuscitation triangle roles ensures that every single compression is a high-quality, life-sustaining one. Mastering these communication skills and team dynamics is what turns a protocol into a successful resuscitation.
Adapting Roles When Your Team Is Small
In a perfect world, a six-person resuscitation team materializes for every cardiac arrest. But we don't work in a perfect world. In the trenches—whether in a small clinic, a rural hospital, or during a chaotic shift—you often have to make do with a much smaller crew.
The good news? The resuscitation triangle roles aren't rigid rules; they're a flexible framework. You can absolutely adapt them for short-staffed situations without compromising care. The key is to combine roles logically, making sure all the critical jobs get done.
Prioritizing and Combining Responsibilities
When you're down a few people, you have to triage the tasks themselves. Your absolute non-negotiables are high-quality compressions, airway management, and defibrillation. These three actions are the bedrock of any successful code. Everything else gets layered on top of these core functions.
Think about the physical layout. The person managing the airway is usually right at the head of the bed, next to the monitor. It’s a natural fit for them to also handle the defibrillator. The Team Leader might have to jump in and help with IV access if no one else is free. It’s all about keeping the essential gears turning, even with fewer hands.
A smaller team doesn't mean a less effective one. It just means every single person needs to be more versatile. You have to be ready to wear multiple hats while keeping communication sharp and staying aware of the entire situation.
How to Combine Roles for Smaller Teams
Adapting on the fly requires a clear, simple plan. The most effective role combinations are built around minimizing movement and reducing cognitive overload. This lets each person focus on a logical group of tasks. For instance, one provider might handle everything at the head of the bed, while another focuses on circulation and medications.
No matter what, protecting the quality of CPR is paramount. A dedicated compressor should always be your top priority if possible. Guideline updates have consistently drilled this home. The 2015 revisions, for example, pushed for a specific compression rate of 100-120 per minute, a narrow window that research has directly linked to better survival rates. You can dig deeper into how these guidelines improve outcomes by exploring the full research on cardiac arrest survival rates.
When you know you'll be working with a skeleton crew, it helps to have a pre-planned strategy for combining roles. Here’s a practical way to think about redistributing responsibilities based on your team's size.
How to Combine Roles for Smaller Teams
Team SizeRole 1 CombinationRole 2 CombinationRole 3 CombinationThree-Person TeamTeam Leader / Recorder (Directs the code and documents events)Compressor / IV/Meds (Performs compressions and administers drugs)Airway / Monitor (Manages airway and operates the defibrillator)Four-Person TeamTeam Leader (Oversees the entire resuscitation effort)Compressor (Focuses solely on high-quality compressions)Airway / IV/Meds (Manages airway and administers drugs)
This kind of structured approach proves that the resuscitation triangle isn't about having a specific number of people in the room. It’s a flexible system designed to bring order to chaos, no matter how big—or small—your team is.
Building and Maintaining Team Proficiency
Mastering the resuscitation triangle roles isn’t a one-and-done deal; it's an ongoing commitment. Think of these life-saving abilities as perishable skills. If you don't use them, you lose them.
A team that doesn’t consistently train together can quickly develop weak spots, leading to hesitation and errors when every single second counts. This is why continuous learning is completely non-negotiable for any high-performance resuscitation team.
The Modern Shift in Medical Education
For years, the general consensus leaned toward the belief that only in-person classes from specific organizations were valid for certification. Let's be clear: that outdated idea is simply no longer true.
The healthcare industry is evolving. Hospitals, clinics, and entire healthcare systems across the country increasingly recognize that high-quality, accredited online education is an effective and powerful alternative for today's busy professionals. In fact, numerous peer-reviewed studies show that online learning leads to knowledge retention and patient care outcomes that are equal or even superior to traditional classroom settings.
Why Online Certification Is Gaining Traction
The move toward online learning isn't just about convenience—it's about equal quality, flexibility, and cost-savings. Modern online certification platforms are built to deliver robust, expert-led training that truly prepares you for real-world chaos.
Here’s why they work so well:
- Unmatched Flexibility: You can learn and get certified on your schedule, without having to take time off work or travel to a training center.
- Cost-Effectiveness: Online courses often cut out the extra costs of travel, printed materials, and classroom fees, making crucial education more affordable.
- Self-Paced Learning: Got a complex topic? You can review it as many times as you need. This is a massive advantage over a rushed, one-day class where you might not fully grasp everything before moving on.
This growing acceptance reflects a broader industry trend. It's an acknowledgment that the quality of education comes from the curriculum and accreditation, not the physical room where it's delivered.
It's also worth remembering that the skills we're talking about operate within a larger system. The groundwork for effective emergency response often comes from broader public health initiatives, which shape the environment our teams work in. The skills you learn in certification are vital, especially when it comes to team dynamics. For a deeper dive, check out our guide on the 5 elements of effective team dynamics in ACLS.
At ProMed, we’re proud to be at the forefront of this shift, providing accredited, convenient, and credible ACLS and PALS certifications aligned with the future of healthcare.
Common Questions about Resuscitation Triangle Roles
When you start putting the resuscitation triangle into practice, a few common questions always seem to pop up. It's one thing to see it on a diagram, but another entirely when you're in the thick of it. Let's tackle some of the most frequent queries to help you feel more prepared for a high-pressure code.
Who Is the Most Important Person on the Team?
This might sound like a cop-out, but every role is absolutely vital. That said, if you had to pick one, the Team Leader is the linchpin holding the entire operation together. Think of them as the conductor of an orchestra.
By staying hands-off, they maintain a crucial bird's-eye view of the whole scene. They're the ones making sure ACLS algorithms are followed, calling out the next steps, and keeping the team moving in sync. Without a clear leader, even a room full of brilliant clinicians can descend into chaos, leading to missed steps and dangerous delays. A great Team Leader turns a group of individuals into a life-saving machine.
How Often Should the Compressor Role Be Switched?
You must switch compressors every two minutes. This isn't a suggestion; it's a hard-and-fast rule. This timing lines up perfectly with the five cycles of 30 compressions and 2 breaths, right before a rhythm check. The swap needs to be lightning-fast—we're talking seconds—to minimize any interruption in blood flow.
Why so strict? Because the data is crystal clear: compressor fatigue is real and it sets in fast, sometimes in as little as one minute. Once fatigue hits, compressions get shallower and slower, no matter how strong the provider is. Mandating a switch every two minutes is a core ACLS principle that ensures the patient gets high-quality CPR from start to finish.
Can Online Courses Truly Prepare You for a Real Code?
Absolutely. The old-school belief that only in-person training counts is quickly becoming a thing of the past. High-quality, accredited online certification courses are now designed to be just as effective as traditional classes for mastering the critical thinking skills needed for resuscitation.
The general consensus in the industry is slowly shifting. More and more hospitals, clinics, and organizations are recognizing that top-tier online training delivers the same educational outcomes but with the accessibility and flexibility that today's demanding schedules require.
These aren't just passive videos. Modern online courses use interactive simulations, instruction from seasoned experts, and detailed clinical scenarios to drill you on the resuscitation triangle roles, algorithms, and split-second decisions you'll face in a real code. It's a credible, effective, and future-focused way to earn and maintain your life-saving certifications.
Ready to master these roles with confidence? ProMed Certifications offers fully accredited, 100% online ACLS, PALS, and BLS courses that fit your schedule. Get certified or recertified with the convenience and quality trusted by thousands of healthcare professionals. Explore our courses today!
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today