Mastering the PALS Cardiac Arrest Algorithm

When you’re in the middle of a pediatric emergency, the last thing you want is confusion. The PALS cardiac arrest algorithm is a critical component of pediatric advanced life support, designed to cut through chaos with clear, evidence-based steps. Think of it as your clinical road map during resuscitation. This guide will help you better equip yourself to navigate these high-stress scenarios with confidence, ultimately improving outcomes for your young patients.
What is the PALS Cardiac Arrest Algorithm?
This guide is built to walk you through every decision point in the PALS cardiac arrest algorithm. It's about more than just memorizing steps; it's about understanding the why behind each action. In a way, it’s the ultimate "how-to guide" for a medical crisis. The same principles that go into creating effective 'how-to guides' apply here—clear instructions save lives.
We’re going to break down why kids need a completely different approach than adults and touch on the key distinctions in resuscitation. Grasping these fundamentals provides the foundation you need to master these life-saving skills.
Why a Specialized Pediatric Algorithm Is Necessary
Here’s the thing: children aren't just tiny adults. Their bodies work differently, and the reasons they go into cardiac arrest are usually worlds apart from what we see in adults. Most adult arrests stem from a primary cardiac event. In kids, it’s almost always a secondary issue, typically caused by respiratory failure or shock. This fundamental difference shapes the entire PALS approach.
The data backs this up. For instance, European data on pediatric cardiac arrests shows that for in-hospital events, the return of spontaneous circulation (ROSC) is between 60% and 72%. That's a huge jump compared to out-of-hospital arrests, highlighting the impact of timely, appropriate care.
There are a few critical reasons we need a pediatric-specific algorithm:
- Different Causes: The algorithm prioritizes treating the common culprits in kids, like respiratory distress and shock.
- Physiological Differences: It's designed to account for smaller airways, faster metabolic rates, and unique fluid needs.
- Equipment and Dosages: Everything is weight-based, from medication doses to the size of the equipment used.
By the time you finish this guide, you'll have a rock-solid understanding of the algorithm, ready to navigate every branch with confidence.
How It Works: The First Two Minutes
When a child goes into cardiac arrest, you're racing against the clock. The PALS cardiac arrest algorithm gives you a universal starting point, no matter the rhythm: start high-quality CPR immediately.
Think of those first two minutes like this: they are the foundation for everything that follows. If the foundation is weak, the entire resuscitation attempt can crumble. The goal is simple but critical: get blood moving to the brain and heart. Flawless CPR isn't just a suggestion; it's non-negotiable.
The Nuts and Bolts of High-Quality Pediatric CPR
For your compressions to make a difference, they have to hit key metrics. Each component works together to maximize blood flow until the heart can beat on its own again.
- Compression Rate: You need to push at a rate of 100-120 compressions per minute. That’s the sweet spot for keeping oxygenated blood circulating.
- Compression Depth: In children, aim for a depth of at least one-third of the chest's front-to-back diameter—about 2 inches (5 cm). For infants, it’s around 1.5 inches (4 cm).
- Full Chest Recoil: This is just as important as the push down. You have to let the chest come all the way back up between compressions to allow the heart to refill with blood.
- Minimal Interruptions: Every time you stop compressions, blood flow plummets. Keep pauses, like when attaching a monitor, under 10 seconds.
This isn't just academic. A major study of 9,664 pediatric in-hospital cardiac arrests found that hospitals with longer average CPR times had a 10% higher survival rate. That kind of real-world evidence shows how vital it is to stick to these guidelines. You can Learn more about the research on CPR duration and survival rates.
While one team member focuses on perfect CPR, another should attach the ECG monitor or defibrillator pads. This is your next priority because the cardiac rhythm is the first major fork in the road. What you see on that monitor dictates every move you make from that point forward.
Managing Shockable Rhythms: VF and pVT
When the monitor shows a chaotic rhythm like Ventricular Fibrillation (VF) or a rapid, ineffective one like pulseless Ventricular Tachycardia (pVT), you've gone down the "shockable" branch of the PALS cardiac arrest algorithm. Think of these as electrical problems. At their core, an electrical shock is often what's needed to fix them.
The first step is recognizing what you're seeing. VF looks like a messy, quivering line. pVT presents as a wide, fast, regular rhythm. In either case, the outcome is the same: the heart isn't contracting effectively, and you won't find a pulse. For these rhythms, defibrillation is your single most important intervention.
The Defibrillation and CPR Cycle
Once your team confirms a shockable rhythm, every action must be quick and coordinated. The treatment follows a specific cycle designed to reset the heart's chaotic signals. Think of it as a powerful one-two punch: an electrical shock followed immediately by high-quality CPR.
Here's the breakdown:
- Deliver a Shock: The starting energy dose for pediatric defibrillation is 2 Joules per kilogram (J/kg).
- Resume CPR Immediately: Don't waste a second. As soon as the shock is delivered, get right back on the chest for two minutes of CPR. This is not the time to check for a pulse. The heart just got a major reset and needs immediate mechanical support.
- Perform a Rhythm Check: Only after two full minutes of CPR do you briefly pause to check the monitor.
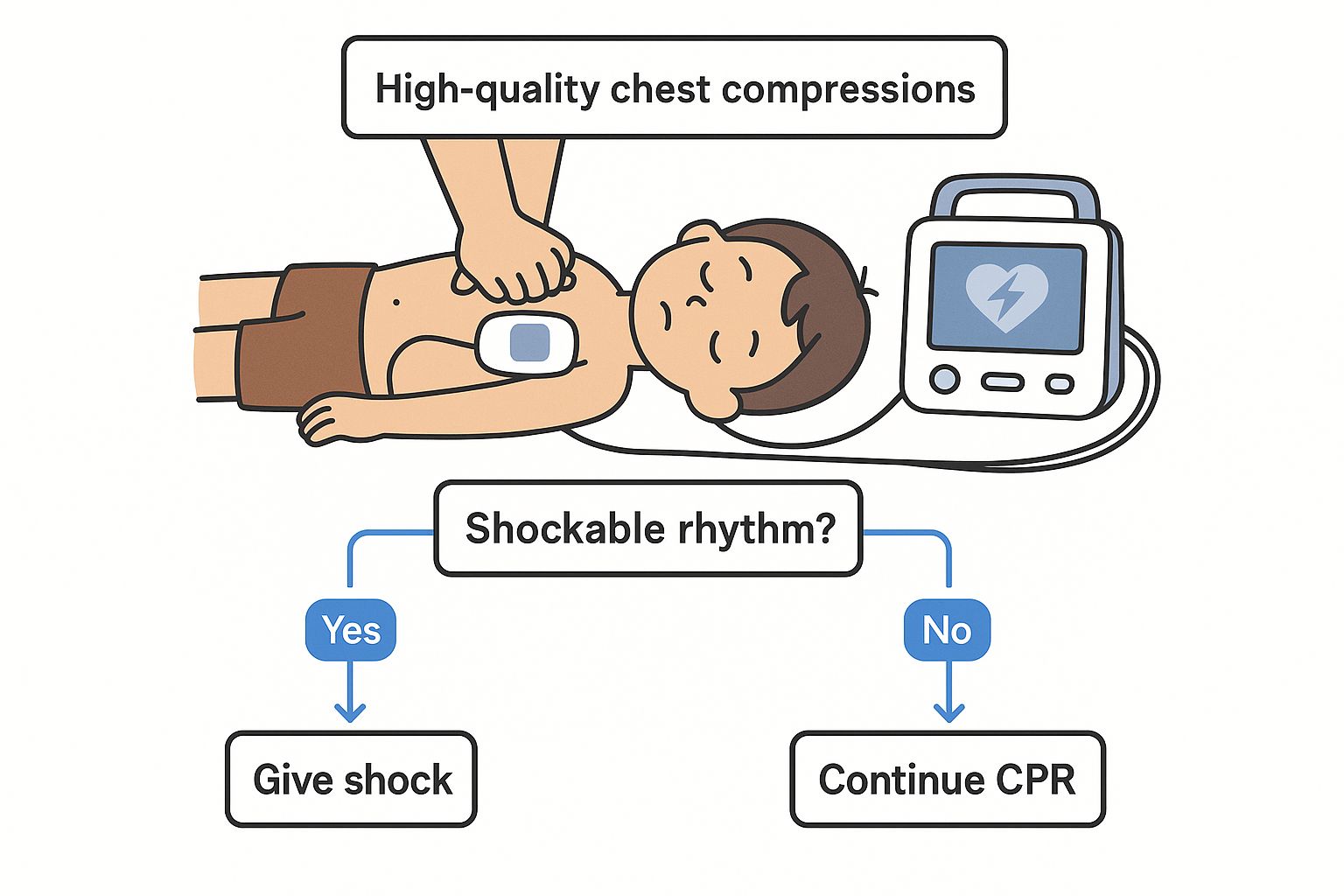
As the diagram shows, the core loop for treating VF and pVT is the immediate delivery of a shock, followed by uninterrupted CPR. If the rhythm is still shockable after that two-minute cycle, you'll deliver another shock—but this time, you'll increase the energy dose.
The second shock should be delivered at 4 J/kg. For any shocks after that, the dose can be increased again, but it should never go above 10 J/kg or the maximum adult dose, whichever is lower. This escalating approach gives you the best chance of converting the rhythm while minimizing potential harm.
Shockable vs Non-Shockable Rhythms in PALS
Understanding these fundamental differences is key to making the right call in the first few seconds of a pediatric code. While the immediate actions differ, both pathways emphasize the critical importance of high-quality CPR and addressing reversible causes.
Managing Non-Shockable Rhythms: Asystole and PEA
When your monitor shows a rhythm that isn't VF or pVT, you’re automatically heading down the other side of the PALS cardiac arrest algorithm. This pathway manages non-shockable rhythms: Asystole and Pulseless Electrical Activity (PEA).
Think of Asystole as the classic "flatline"—a straight line on the monitor, meaning no electrical activity. PEA is a bit more deceptive. The monitor shows organized electrical activity, but when you check the patient, there's no pulse.
In either scenario, the takeaway is the same: defibrillation will not work. These aren't electrical problems that a shock can fix, so hitting the shock button is futile.
The CPR and Epinephrine Cycle
Instead of reaching for the defibrillator, your priorities shift to two key interventions: continuous, high-quality CPR and timely administration of epinephrine. The goal is to manually generate blood flow to the heart and brain, giving the body the best possible chance to restart.
This side of the algorithm is a straightforward, repeating two-minute loop:
- Resume High-Quality CPR: Uninterrupted chest compressions are your absolute top priority.
- Administer Epinephrine: As soon as you have IV or IO access, give 0.01 mg/kg of epinephrine. You'll repeat this dose every 3 to 5 minutes.
- Rhythm and Pulse Check: After two full minutes of CPR, you'll briefly pause to check the monitor and feel for a pulse.
This cycle is the backbone of your response. While it's running, the team should simultaneously be hunting for and treating any reversible causes (the H's and T's). It’s a sobering fact that the initial rhythm heavily influences the outcome. Asystole is found in 82-95% of pediatric arrests and carries a much lower survival rate than VF. This is why following the algorithm is so crucial—it ensures the right interventions are applied without delay. You can dive deeper into how epidemiological factors influence PALS guidelines on pmc.ncbi.nlm.nih.gov.
A solid understanding of the distinct steps for both shockable and non-shockable rhythms is non-negotiable. For a complete overview, check out our detailed guide on the pediatric cardiac arrest algorithm for more information.
Key Medications in the PALS Algorithm
In a pediatric code, medications are a powerful part of your toolkit. They run in parallel with CPR and defibrillation, working to give the heart the best chance to restart a healthy rhythm. But here’s the most important thing to remember: meds should never cause a significant pause in chest compressions. Every second without perfusion counts.
Before you push any drugs, you need reliable access. An IV is great, but if you can't get one quickly, don't hesitate to go for an intraosseous (IO) line. Wasting minutes trying for a tricky IV is a classic mistake.
Medications for Shockable Rhythms
For shockable rhythms like VF and pVT, drugs come into play after initial shocks haven't worked. The goal is to make the heart more responsive to the next defibrillation attempt.
- Epinephrine: This is your go-to vasopressor. It tightens blood vessels, pushing more blood to the heart and brain. You'll give the first dose after the second shock. The dose is 0.01 mg/kg, repeated every 3 to 5 minutes.
- Amiodarone: This is your first choice. It works to stabilize the heart's chaotic electrical firing. The initial dose is a 5 mg/kg bolus.
- Lidocaine: If amiodarone isn't available, lidocaine is your backup. The starting dose is 1 mg/kg.
Medications for Non-Shockable Rhythms
When you're dealing with Asystole or PEA, your medication strategy is much simpler. Defibrillation is off the table, so your focus shifts to making your CPR as effective as possible.
Epinephrine is the absolute cornerstone for treating non-shockable pediatric cardiac arrest. Its main job is to boost coronary and cerebral perfusion pressure, creating a better internal environment for the heart to potentially achieve Return of Spontaneous Circulation (ROSC).
The process is direct: give epinephrine 0.01 mg/kg as soon as you have IV/IO access. From there, you just keep giving that same dose every 3 to 5 minutes. That’s it. No other drugs are routinely recommended unless you've identified a specific reversible cause (like giving naloxone for a suspected opioid overdose).
Finding And Treating Reversible Causes
Running a successful PALS code is about more than just mastering CPR and knowing drug dosages. It’s about being a detective. You have to constantly ask why the arrest happened, and this needs to happen in parallel with every other action.
Think of it this way: while your team is pushing meds and managing the airway, a part of your brain must hunt for the root cause. Often, the key to getting a pulse back—Return of Spontaneous Circulation (ROSC)—isn't another dose of epinephrine. It's fixing the one thing that made the heart stop. This is where the H's and T's come in.
Unpacking The H's and T's Mnemonic
The H's and T's are a simple, powerful mnemonic to help you recall the most common—and correctable—causes of pediatric cardiac arrest. As you move through each two-minute cycle of CPR, you should be mentally running through this checklist.
The "H's" cover the patient's internal state:
- Hypovolemia: Is the tank empty? Look for poor perfusion or a history of vomiting, diarrhea, or bleeding.
- Hypoxia: This is a huge one in kids. Is the airway patent? Are ventilations effective? Is the child getting enough oxygen?
- Hydrogen Ion (Acidosis): A severely acidotic heart won't respond well to interventions. Think about causes like DKA or prolonged poor perfusion.
- Hypo/Hyperkalemia: Are the electrolytes out of whack? A history of renal failure can be a major clue.
- Hypoglycemia: Low blood sugar is a classic and easy fix. Always get a glucose level.
- Hypothermia: Was the child found in a cold environment? A child isn't dead until they are warm and dead.
The "T's" cover "plumbing" and external problems:
- Tension Pneumothorax: This needs a mechanical fix, now. Look for absent breath sounds on one side.
- Tamponade (Cardiac): Is fluid squeezing the heart? Consider this with a history of heart surgery or chest trauma.
- Toxins: Could the child have ingested something? Check the scene for clues and ask caregivers pointed questions.
- Thrombosis (Pulmonary or Coronary): While less common in kids, a blood clot can still be the underlying cause.
Integrating Treatment Into The Algorithm
When you identify a reversible cause, you must act immediately. For instance, if you suspect hypovolemia, get a fluid bolus of normal saline or lactated Ringer's solution (20 mL/kg) in as fast as you can.
The search for reversible causes isn’t a passive step. It's an active, ongoing investigation that you weave into every cycle of the PALS algorithm. It’s what turns resuscitation from a rigid protocol into a responsive, targeted intervention.
PALS Reversible Causes The H's and T's
This table provides a detailed breakdown of the common reversible causes of pediatric cardiac arrest, their potential signs, and the immediate corrective actions as per the PALS guidelines.
By systematically thinking through these possibilities during every pause, you give your patient the absolute best shot at a good outcome.
Care After Return of Spontaneous Circulation (ROSC)
Getting ROSC is a massive win, but the work is far from over. What you do next is just as critical for giving that child the best long-term outcome. Your focus now pivots from restarting the heart to protecting the brain and other vital organs. Think of it like this: you've just pulled the child from a fire, and now you have to start assessing and preventing further damage. This is post-resuscitation care.
Key Goals in Post-Resuscitation Care
The priorities in the post-ROSC phase are clear and systematic. You’ll be juggling multiple body systems at once to give your patient the best shot at a full recovery.
Here’s what you need to zero in on:
- Optimizing Ventilation and Oxygenation: Maintain a patent airway and use ventilatory support to keep oxygen saturation between 94-99%. Both too little (hypoxia) and too much (hyperoxia) oxygen can cause harm.
- Managing Hemodynamics: Keep a close eye on blood pressure. You'll likely use IV fluids or vasopressors to maintain a systolic blood pressure appropriate for the child's age, ensuring adequate organ perfusion.
- Controlling Temperature: Targeted Temperature Management (TTM) is a game-changer for neuroprotection. The goal is to maintain a core temperature between 32°C and 36°C for at least 24 hours to help the brain recover.
- Monitoring and Treating Seizures: Seizures are common after cardiac arrest and can worsen a brain injury. Continuous EEG monitoring is often used to catch any seizure activity as soon as it starts.
Every step requires meticulous management and thorough documentation. In any critical care scenario, improving clinical documentation is a cornerstone of effective teamwork and patient safety.
For a much deeper dive into this vital phase of care, check out our complete guide to post-cardiac arrest care.
PALS Algorithm Frequently Asked Questions
Even with a clear algorithm, practical questions are bound to pop up in a high-stress resuscitation. Let's tackle some of the most common queries about the PALS cardiac arrest algorithm.
What Is the Correct Escalating Energy Dose for Defibrillation?
For shockable rhythms like VF and pVT, the game plan is to start low and escalate methodically.
- Your initial shock should be 2 Joules per kilogram (J/kg).
- If that doesn't work, after two more minutes of CPR, your second shock will be 4 J/kg.
- For any subsequent shocks, you can increase the energy, but never go above a maximum of 10 J/kg or the standard adult dose—whichever is lower.
What Is the Maximum Single Dose for Key Medications?
Knowing your medication limits cold is critical. The two most common drugs in the PALS cardiac arrest algorithm have hard caps on their single doses, no matter the child's weight.
- Epinephrine: The max single dose is 1 mg.
- Amiodarone: The max single dose is 300 mg.
These limits are in place to prevent toxicity and other dangerous side effects.
How Does the PALS Algorithm Differ for Infants vs. Children?
The core principles of the PALS cardiac arrest algorithm are the same for infants (under 1 year) and children. The fundamental steps don’t change. However, the practical application, especially CPR technique, does.
For infants, you'll use the two-finger or two-thumb encircling hands technique. The target depth is about 1.5 inches (4 cm). For children, you’ll switch to one or two hands to get the necessary depth of about 2 inches (5 cm). All medication and defibrillation doses remain weight-based.
New tools are making a huge difference for healthcare professionals looking to build muscle memory. For example, Virtual Reality for Medical Training provides a safe, immersive environment to practice these complex skills without real-world risk.
This guide should lay the framework for understanding the PALS cardiac arrest algorithm. Mastering these life-saving skills is a continuous journey. At ProMed Certifications, we provide accredited, online PALS courses designed to fit your demanding schedule, helping you stay sharp and ready for any pediatric emergency. Enroll today and get certified with confidence.
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today