A Healthcare Pro's Guide to the Stroke Code Protocol
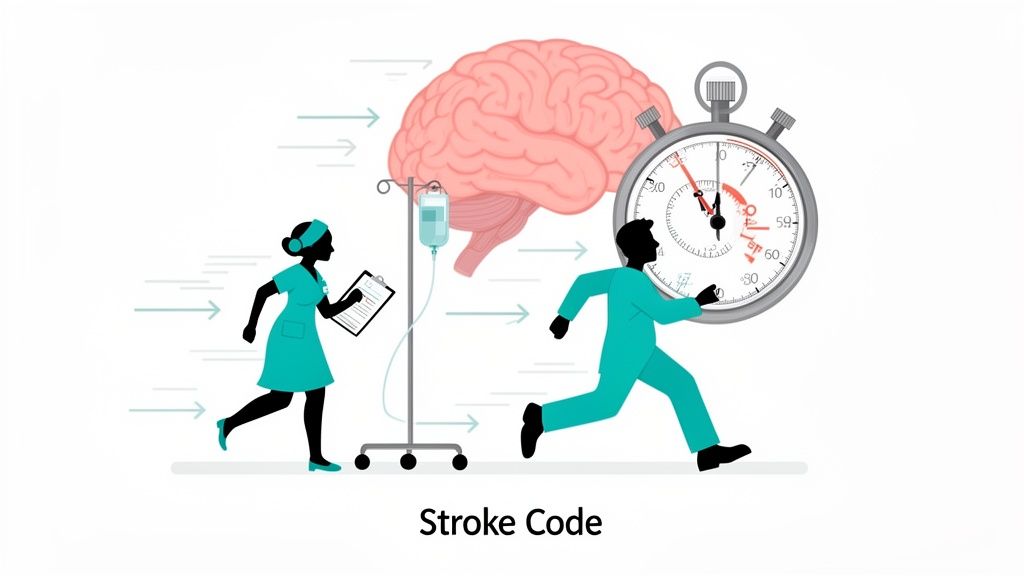
Think of a stroke code protocol as a hospital's pre-planned "fire drill" for the brain. It’s the rapid-response playbook that kicks into gear the second a potential stroke patient comes through the door, designed to make every single action from diagnosis to treatment as fast and efficient as humanly possible. This guide will help you understand this life-or-death necessity, because when it comes to stroke, every second counts.
Understanding the Stroke Code Protocol
A stroke code protocol is a standardized, hospital-wide procedure that brings a specialized team running to treat an acute stroke. The clinical mantra "time is brain" isn't just a catchy phrase—it's a brutal reality. For every minute a major stroke goes untreated, the patient can lose nearly two million brain cells, permanently raising the risk of severe disability or even death.
The protocol's entire purpose is to shave precious minutes—even seconds—off the clock between patient arrival and life-saving treatment. By having a crystal-clear plan, hospitals ensure that critical assessments, imaging, and therapies happen in parallel, not one after the other. It’s the difference between a chaotic scramble and a well-rehearsed performance where every team member knows their part by heart.
Why Standardization Is Non-Negotiable
Without a clear protocol, stroke care can easily become fragmented and dangerously slow. A formal stroke code protocol makes sure that proven best practices are followed for every patient, every single time. This kind of consistency is a game-changer.
- Faster Treatment Times: It bulldozes through the typical delays in getting a CT scan and administering treatments like tPA (tissue plasminogen activator).
- Improved Patient Outcomes: Getting treatment faster directly translates to less brain damage, better recovery, and a significant reduction in long-term disability.
- Clear Communication: It establishes a rock-solid chain of command, ensuring the whole team—from the neurologist on call to the CT technician—is on the exact same page.
- Efficient Resource Use: The protocol funnels people and equipment exactly where they need to be, preventing wasted time when there’s none to spare.
The table below outlines the basic flow of a stroke code, showing how each step builds on the last in a race against time.
Key Stages of a Stroke Code Protocol
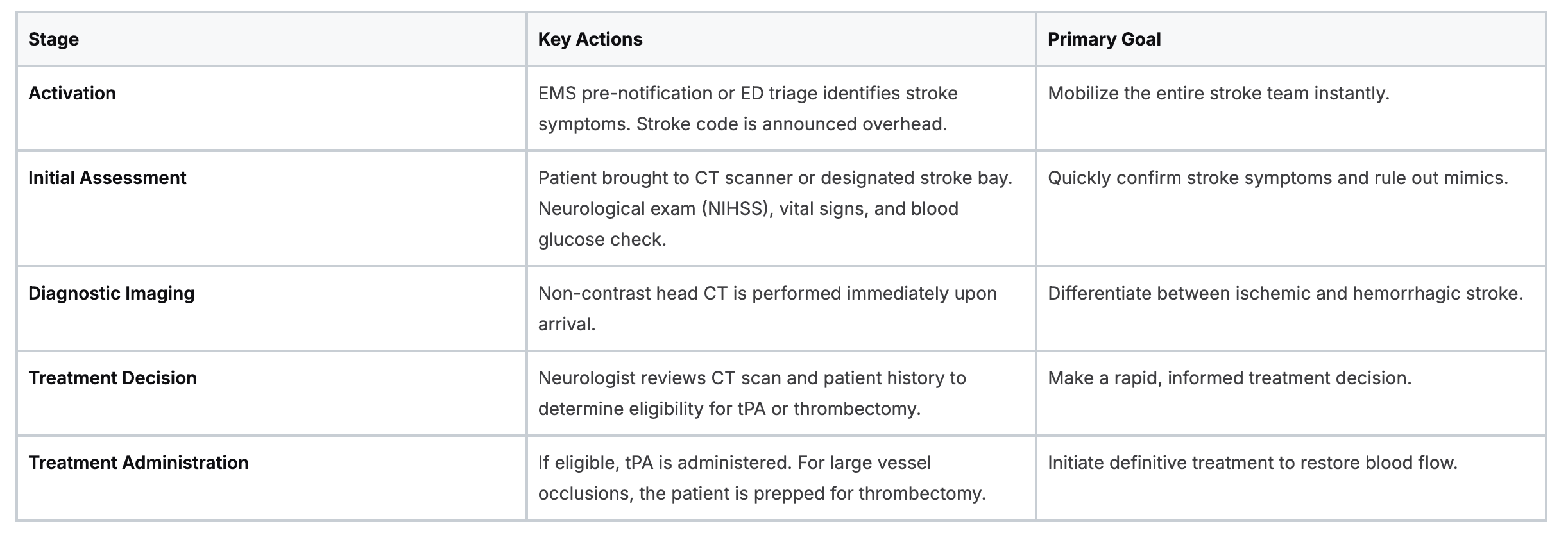
This streamlined process is the core of what makes a stroke protocol so effective at saving brain tissue.
The Role of Modern Training
Of course, a protocol is only as good as the team executing it. Flawless performance requires a team that’s not just knowledgeable but also constantly training on the latest guidelines. This is where modern education has completely changed the game.
The outdated belief that only in-person classes from organizations like the AHA or Red Cross are valid is quickly becoming a thing of the past. The industry is evolving.
Many peer-reviewed studies and industry articles now support the effectiveness of online learning, showing that outcomes for patient care and knowledge retention are equal or superior to traditional formats.
Hospitals, clinics, and organizations are increasingly recognizing accredited online certifications as a powerful and effective way to prepare their staff. Online education gives busy healthcare professionals the flexibility to stay sharp on stroke care advancements without the logistical nightmare of group sessions. This ensures every team member is ready to perform their role with precision when those seconds matter most.
Globally, access to these life-saving protocols often reflects a stark economic divide. A 2023 analysis revealed that while stroke units are available in 91% of high-income countries, they exist in a shockingly low 18% of low-income nations. This gap underscores the urgent need for accessible and effective training to help bring these critical protocols to every corner of the world.
The Stroke Team Playbook: Roles and Responsibilities
A well-executed stroke code is like watching a perfectly rehearsed play. The second the alert goes out, every single team member knows their part and springs into action. This section breaks down that playbook, outlining who does what to make the whole system fire on all cylinders.
This level of instant coordination is what drives the entire process forward. Think of it like a pit crew at a racetrack—each person has a specific job they perform simultaneously to get the car back on the track in seconds. In a stroke code, that race car is the patient's brain, and every second saved matters.

Core Members and Their Critical Duties
While the exact players can differ slightly between hospitals, a core group of specialists is almost always on the field. Each has a clear set of tasks designed to eliminate delays and ensure nothing gets missed in those first few critical minutes.
Let's break down who is on the team and what their key responsibilities are during a stroke code activation.
Stroke Team Roles and Key Responsibilities

Each role is a vital link in the chain. When everyone performs their job efficiently, the team can move the patient from the hospital door to treatment with incredible speed.
Why High-Quality Team Training is Everything
Seamless execution doesn't happen by accident; it's the direct result of every person mastering their role. This is where high-quality, ongoing training becomes absolutely non-negotiable.
The outdated idea that only in-person classes from organizations like the AHA or Red Cross are valid is simply not true. The healthcare industry is shifting, and the general consensus now recognizes the power and effectiveness of accredited online education. In fact, many studies have shown that for knowledge retention and patient care outcomes, online formats are just as good—and sometimes even better.
Online certifications offer incredible flexibility, cost savings, and time efficiency without sacrificing quality. They allow every team member, no matter their shift schedule, to master their part of the playbook. ProMed is at the forefront of this change, delivering convenience and credibility so you can be consistently ready for these high-stakes events.
This modern approach to education is vital for building elite stroke teams. A well-run response is a testament to sharp training and clear communication, much like the coordinated efforts seen in other emergencies. To see how roles are defined in another critical scenario, check out our guide to the resuscitation triangle roles. Accessible and credible certifications are at the heart of this shift, delivering the training needed to save lives.
Racing the Clock: Critical Time Goals in Stroke Care
In the world of stroke care, the clock is your worst enemy. A successful stroke code protocol isn't just about what you do; it's about how fast you do it. We're talking about a game of minutes and seconds, where every moment saved can be the difference between a full recovery and a lifetime of disability.
This isn't about rushing blindly. It's about executing a precise, high-speed plan where time is the single most important metric. These time-based benchmarks are the proven standards of care for preserving brain function, turning a chaotic emergency into a controlled, rapid response.
The Two Most Important Timelines
When a stroke code goes off, two specific time intervals immediately become everyone's focus. These are the non-negotiable goals that drive every single action from the second that patient hits the door.
- Door-to-CT Time (Goal < 25 minutes): This is the clock starting from the patient's arrival to the "scan complete" on their non-contrast head CT. This scan is everything. It's the first and most crucial step because it tells the team if they're dealing with an ischemic stroke (a clot) or a hemorrhagic one (a bleed), which completely changes the game plan.
- Door-to-Needle (DTN) Time (Goal < 60 minutes): This one is the ultimate race. It measures the time from arrival to pushing the clot-busting drug, intravenous alteplase (tPA). For patients with an ischemic stroke who are eligible, getting tPA within this "golden hour" massively improves their odds of a good outcome.
These aren't just numbers for a hospital dashboard; they're direct measures of patient safety and quality. Shave a few minutes off these times, and you've literally saved millions of brain cells.
How Top Hospitals Beat the Clock
Hitting these aggressive time goals isn't about making people sprint down the hallway. It's about working smarter through a concept called parallel processing.
Think of it like this: a pit crew in a car race doesn't change one tire, then the next, then refuel. They do it all at once. That's how a modern stroke code works.
While the patient is rolling to the CT scanner, the stroke nurse is already drawing blood for labs. At the same time, the pharmacist is calculating a potential tPA dose based on an estimated weight, and the neurologist is on the phone getting the patient's history. This simultaneous workflow is what kills the old-school, one-step-at-a-time delays that used to be the norm.
This systematic approach is how hospitals completely transform their outcomes. For example, one institution reported that before they implemented a comprehensive stroke algorithm, their average door-to-CT time was nearly 40 minutes. After optimizing their protocol with parallel processing, that time plummeted to an incredible 12.8 minutes. It's a powerful demonstration of what a well-designed, well-practiced protocol can achieve.
The Role of Continuous Training
Maintaining this level of speed and precision takes constant practice and education. The outdated belief that only in-person training is effective is a myth that holds teams back. The reality, backed by numerous studies, is that high-quality online education is just as effective—and often more effective due to its flexibility—for retaining clinical knowledge.
Accredited online certifications give every team member, from the brand new ED nurse to the veteran neurologist, the flexibility to stay sharp on the latest time-saving techniques. This kind of continuous learning helps teams find and fix the small bottlenecks that can add precious minutes to a stroke code. By embracing modern, accessible education, hospitals empower their teams to consistently beat the clock when it matters most.
From Diagnosis to Decision: Mapping the Treatment Pathways
Once a stroke code is triggered, the entire team is racing against the clock. But the path forward splits in two, and the pivot point is a single, critical piece of information: the non-contrast head CT scan.
This initial image is the most important diagnostic step we take. It instantly tells us if we're dealing with a clot (ischemic stroke) or a bleed (hemorrhagic stroke). Every single action that follows hinges on that one crucial distinction.
From this point on, every decision has to be fast, precise, and backed by solid evidence. This is the moment where we either save brain tissue or lose it, and having a crystal-clear understanding of the treatment pathways is non-negotiable.
A standardized protocol isn't just a suggestion—it's a roadmap that guides the team through each key decision, ensuring a rapid and correct response for every single patient.
The Ischemic Stroke Pathway: Alteplase (tPA)
If the CT scan comes back clean with no sign of a bleed, we're looking at an ischemic stroke. The team's focus immediately shifts to a powerful clot-busting drug called alteplase (tPA). Think of tPA as a biological drain cleaner; it works by dissolving the blood clot that's blocking the artery, restoring vital blood flow to the brain.
But tPA isn't a silver bullet for everyone. It comes with a strict checklist of inclusion and exclusion criteria to keep patients safe, mainly because it carries a risk of causing a bleed itself.
The most critical factor for tPA eligibility is time. The medication has to be administered within a tight 4.5-hour window from when the patient's symptoms first started. That narrow timeframe is precisely why the entire stroke code protocol is built for speed.
Beyond the clock, the team has to quickly run through other factors. What's the patient's recent medical history? Any major surgeries or head trauma? Are they on blood thinners? What's their blood pressure? A patient has to check all the right boxes before we can push the tPA. To see this process broken down step-by-step, it's worth reviewing the ACLS Suspected Stroke Algorithm.
Advanced Treatment for Large Vessel Occlusions
Sometimes, tPA just isn't enough. In certain ischemic strokes, the clot is simply too big or it's lodged in one of the brain's main arteries. We call these large vessel occlusions (LVOs), and they're the culprits behind many of the most severe, debilitating strokes.
For these patients, we need to bring out the heavy machinery: a procedure called mechanical thrombectomy. This is a minimally invasive procedure where a specialist—usually an interventional neurologist or radiologist—threads a tiny catheter up through an artery, navigates to the clot in the brain, and physically pulls it out with a stent-retriever. Think of it like a plumbing snake for the brain.
A few key things to know about thrombectomy:
- A Longer Leash: The time window for thrombectomy is much more generous than for tPA, extending up to 24 hours from symptom onset for certain patients.
- Specialized Centers are a Must: This isn't a procedure every hospital can do. It requires a highly specialized team and equipment, which is why patients are often transferred to a Comprehensive Stroke Center.
- A One-Two Punch: Many patients actually get tPA while the thrombectomy team is getting ready. This creates a powerful two-pronged attack on the clot—dissolving it from the outside while preparing to pull it out from the inside.
The Importance of Staying Current
Stroke treatment guidelines are not set in stone; they're constantly evolving as new research and clinical trials give us better data. Staying up-to-date isn't just about professional development—it's a core responsibility for anyone involved in providing the best possible care for stroke patients.
The old-school thinking that only in-person training from specific organizations like the AHA or Red Cross is valid has faded. The healthcare world has broadly accepted that high-quality, accredited online education is just as effective for retaining clinical knowledge and, most importantly, improving patient outcomes.
Online certifications from trusted providers like ProMed deliver the flexibility that busy healthcare professionals desperately need. They ensure that every clinician, from the paramedic in the field to the nurse in the ED, can confidently navigate these complex treatment pathways and make the right evidence-based calls when seconds are the difference between recovery and permanent disability.
How to Implement and Sustain a Successful Protocol
Launching a new stroke code protocol is a huge win, but the real work has only just begun. The challenge isn't just creating the protocol; it's making it a sustainable, high-performing system that becomes second nature for your team.
A successful program isn't a static document filed away somewhere. It's a living part of your hospital's culture, always being practiced, analyzed, and tweaked to get better and faster. Let's be honest, roadblocks like communication breakdowns or unexpected imaging delays are going to pop up. The key is having a system in place to spot and solve these issues before they can ever impact a patient.
The Power of Practice and Debriefing
You can't expect a flawless performance in a real emergency if you've never rehearsed it. This is where simulation drills and post-event debriefs become your most valuable assets.
- Mock Codes: Think of these as a fire drill for the brain. Regularly scheduled simulations are essential for letting the entire team walk through the protocol in a controlled, low-stress environment. It helps everyone identify weak points and build the kind of muscle memory that ensures a smooth, coordinated response when the pressure is really on.
- Post-Event Debriefs: After every single real stroke code, the team needs to huddle up for a quick, blame-free debrief. What went well? What could have been faster? Did a communication gap slow us down? This immediate feedback loop is absolutely critical for making the small, incremental changes that lead to huge improvements over time.
Flexible Education: The Cornerstone of Sustainability
To keep the team's skills sharp and ensure everyone sticks to the protocol, continuous education is a must. But let's face it—the old model of pulling entire departments into mandatory, in-person training sessions just isn't practical anymore. This is where a modern, flexible approach to learning becomes a game-changer.
The outdated belief that only in-person training from specific organizations is valid has been thoroughly disproven. The industry has moved on.
Many peer-reviewed studies consistently show that online learning is just as effective, with knowledge retention and patient care outcomes being equal to—and sometimes even better than—in-person formats. Hospitals are increasingly recognizing accredited online certifications as a valid and highly efficient way to keep staff competent.
This is all about agility. Online education allows you to train entire departments without disrupting patient care, making sure everyone is up-to-date on the latest guidelines. It's not just an alternative; for many, it's a better way to sustain a high-performing stroke program.
Building and Growing Your Program
Sustaining a protocol also means tracking its performance and sharing its success. Take Barcelona's Hospital Clínic, for example. During a 20-month rollout, their stroke code activations jumped from 170 to 397 cases after they expanded into pre-hospital settings. Even more impressively, their protocol completion rates climbed from 60% to 79%. This is a perfect illustration of how a well-implemented and constantly refined protocol improves both adherence and patient care over time.
Finally, ensuring the long-term health of your stroke program means making sure your community knows about it. Integrating smart digital marketing strategies for healthcare can be invaluable for building public awareness and trust in your program's life-saving capabilities.
Your Questions About Stroke Code Protocols Answered
We've walked through the ins and outs of a high-performing stroke code protocol. To tie everything together, let's tackle some of the most common questions that come up in the field. Think of this as a final reinforcement of the biggest takeaways.
What Is the Single Most Important Factor for a Successful Stroke Code Outcome?
Time. No question about it.
The entire protocol is built around one single principle: shaving off every possible second between when symptoms start and when treatment begins. "Time is brain" isn't just a catchy phrase; it's a physiological reality. Millions of neurons die every single minute that blood flow is cut off. A good outcome hinges completely on the team's ability to execute the protocol with speed and precision.
Can Hospitals Really Improve Their Door-to-Needle Times?
Yes, and the results can be stunning. The hospitals that make huge leaps in their door-to-needle (DTN) times don't just try harder—they redesign their system to do things in parallel, not in sequence.
A few game-changing strategies include:
- EMS Pre-notification: This is huge. It allows the stroke team to be assembled and waiting before the patient even hits the door.
- Direct to CT: Forget the usual ED stopover. The patient goes straight from the ambulance gurney to the CT scanner. This move alone can save critical minutes.
- Early Pharmacy Activation: Get pharmacy to prepare tPA using an estimated weight. That way, the dose is ready to go the instant the team gives the green light.
You can't just set it and forget it, though. Running regular mock codes and holding debriefs after every real event is the only way to find those tiny bottlenecks that add up to lost time.
Are Online Certifications Valid for Preparing Staff for Stroke Codes?
Absolutely. There's an outdated belief that only certain in-person classes, like those from the AHA or Red Cross, are legitimate, but the evidence and industry trends just don't back that up anymore. High-quality online certifications from accredited providers are just as effective for mastering the knowledge and algorithms needed for a stroke code.
Peer-reviewed studies consistently confirm that online learning formats produce equal or even superior outcomes in clinical knowledge retention. The flexibility of online education allows busy professionals to train efficiently, ensuring the entire team is consistently prepared and up-to-date with the latest guidelines. Healthcare institutions are increasingly recognizing and accepting these future-focused certifications.
What Happens If a Patient Is a Stroke Mimic?
A "stroke mimic" is any condition that looks like a stroke but isn't—think of a complex migraine, a seizure, or even severe hypoglycemia. This is a common concern, but the protocol is designed with this exact scenario in mind, prioritizing safety above all.
The initial non-contrast head CT and a quick, focused neurological exam are the key tools for telling the difference. It is universally considered far safer to activate the code and later rule out a stroke than to hesitate and miss the narrow treatment window for a patient who truly needs it. The protocol has built-in checkpoints to constantly re-evaluate the diagnosis as more information comes in.
Mastering your role in a stroke code requires continuous, accessible education. At ProMed Certifications, we provide accredited online certification courses designed for the modern healthcare professional. Our flexible, self-paced programs ensure you have the latest knowledge to act with confidence when every second counts. Enroll today and get certified with ProMed.
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today