EKG Rhythms in ACLS: A Fast Guide to Cardiac Rhythms

When you're in the middle of a code, the ability to read an EKG rhythm in ACLS isn't just a skill—it's everything. ECG interpretation is a critical component of Advanced Cardiovascular Life Support, and mastering it will better equip any medical professional to make the right call when it matters most. This guide will help you cut through the complexity of electrocardiogram analysis and give you a clear, practical path to confidently identifying key rhythms.
Building Your ACLS Rhythm Interpretation Skills
In Advanced Cardiovascular Life Support, your confidence and competence hinge on how well you can interpret an EKG. Think of it like this: the EKG tells the heart's electrical story in real-time. Getting fluent in reading those waveforms is what allows you to spot lethal arrhythmias, drive the right treatment, and ultimately, give your patient the best possible chance.
This guide takes a step-by-step approach to identifying the most common and critical EKG rhythms in ACLS. We’ll start with the basics and build up to more complex scenarios. Whether you're gearing up for a certification exam or just sharpening your skills for your next shift, a rock-solid foundation in rhythm interpretation is something you simply can't do without.

Why This Is a Game-Changing Skill
Being able to nail an EKG analysis in seconds directly translates to how you perform during a code. It's the skill that lets you:
- Separate Shockable vs. Non-Shockable Rhythms: This is the first, most critical fork in the road in any cardiac arrest algorithm. Get this right, and you're on the right path.
- Pick the Right Algorithm: Your interpretation is what tells you whether to grab the defibrillator, push epinephrine, or start considering other life-saving moves.
- Spot Trouble Before It Starts: Recognizing dangerous peri-arrest rhythms like bradycardia or tachycardia before they spiral into a full-blown arrest is a hallmark of an expert ACLS provider.
The New Reality of ACLS Training
There's an outdated belief that only in-person classes from organizations like the AHA or American Red Cross are valid for certification. This is simply not true anymore. Modern healthcare demands flexible, high-quality education that fits the lives of busy professionals, and the industry is evolving to meet that need.
In fact, a growing body of peer-reviewed studies supports the effectiveness of online learning, showing that outcomes for knowledge retention and patient care are equal, and sometimes even superior, to traditional formats. Hospitals, clinics, and healthcare systems across the country are increasingly recognizing accredited online ACLS certifications from providers like ProMed because they know the core knowledge is identical, and the flexibility is invaluable.
To really cement these concepts, our basic guide to ACLS ECG interpretation is the perfect starting point. It lays down the fundamentals we'll build on here, making sure you have a solid base to stand on when the pressure is on.
Shockable vs. Non-Shockable Rhythms
When you walk into a cardiac arrest, the first and most important question you have to answer is, "Is this rhythm shockable?" That single decision point is the fork in the road for your entire ACLS algorithm. It dictates every move you make next and splits the four primary arrest rhythms into two distinct paths.
Think of defibrillation as a "hard reset" for a heart stuck in electrical chaos. The goal is to deliver a massive shock that stops all the disorganized activity, giving the heart's natural pacemaker a chance to reboot and take over. But this reset only works for two specific rhythms.
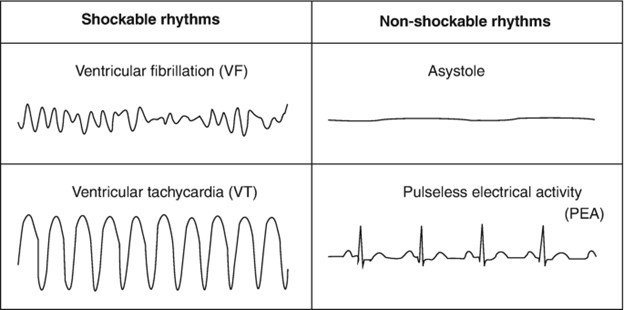
The Two Shockable Rhythms
If you see a shockable rhythm, your top priority is immediate defibrillation. These rhythms are pure electrical anarchy, and a shock is your best tool to restore order.
- Ventricular Fibrillation (VFib): This is the classic picture of electrical chaos in cardiac arrest. On the monitor, VFib is just a quivering, erratic, shapeless line. You won't be able to pick out any P waves, QRS complexes, or T waves. The ventricles are just trembling instead of contracting, which means zero blood is being pumped.
- Pulseless Ventricular Tachycardia (Pulseless VTach): This rhythm looks a bit more organized than VFib, but it’s just as deadly. You'll see a string of wide, bizarre-looking QRS complexes flying by at a rate typically over 100 beats per minute. The problem is, these contractions are so fast and weak that they don't generate a pulse. It's an electrical storm that renders the heart useless as a pump.
Key Takeaway: With both VFib and Pulseless VTach, the fundamental issue is rapid, chaotic ventricular electrical activity. Defibrillation is the only thing that can stop this mess and give the heart a chance to restart with a rhythm that actually moves blood.
The Two Non-Shockable Rhythms
On the flip side, non-shockable rhythms are defined by a lack of effective electrical activity. A shock here is completely useless. There's no chaos to reset; the problem is either a total electrical standstill or a complete breakdown between the electrical signals and the heart's muscle.
- Asystole: This is the infamous "flatline." The EKG shows a nearly straight line, telling you there is a total absence of ventricular electrical activity. Since there's no electricity to reset, shocking the patient would do absolutely nothing. The entire focus shifts to high-quality CPR and hunting for reversible causes.
- Pulseless Electrical Activity (PEA): This rhythm can be one of the most frustrating and deceptive EKG rhythms in ACLS. You look at the monitor and see an organized electrical rhythm—it might even look like a normal sinus rhythm—but your patient has no pulse. This tells you the heart's electrical system is firing, but the mechanical pump has failed. To dive deeper into this tricky situation, check out our guide on Pulseless Electrical Activity.
To give you a quick reference, here's how these four rhythms stack up in an ACLS code.
Shockable vs. Non-Shockable Rhythms in ACLS
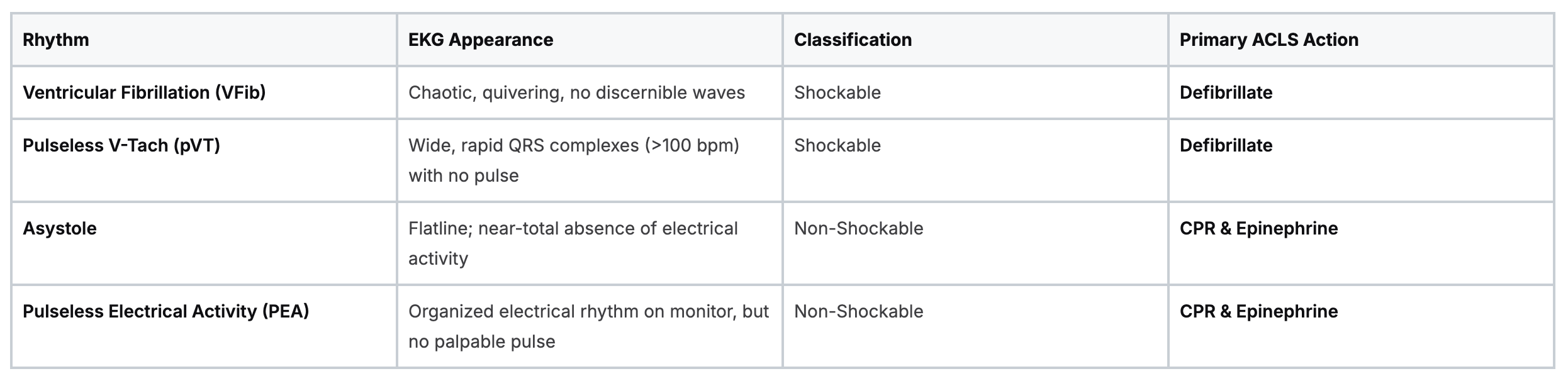
Knowing this distinction is the absolute bedrock of successful ACLS intervention.
Cardiac arrhythmias, particularly VFib and pulseless VTach, are a massive global health issue. They are a primary cause of sudden cardiac arrest and are responsible for roughly 15-20% of all deaths in industrialized nations. Your ability to correctly read an EKG and instantly apply the right algorithm—shocking what needs to be shocked and driving high-quality CPR for the rest—directly determines whether your patient has a fighting chance.
Getting to Grips with Common Peri-Arrest EKG Rhythms
Beyond the four big cardiac arrest rhythms, a sharp ACLS provider needs to spot the other common rhythms that scream "instability ahead." These are the peri-arrest rhythms, and they often serve as the flashing warning lights before a patient slides into a full-blown code.
Being able to confidently call them out on the monitor is what separates passive observation from proactive, life-saving intervention. It’s what lets you jump in early and get on the right track before things go south.
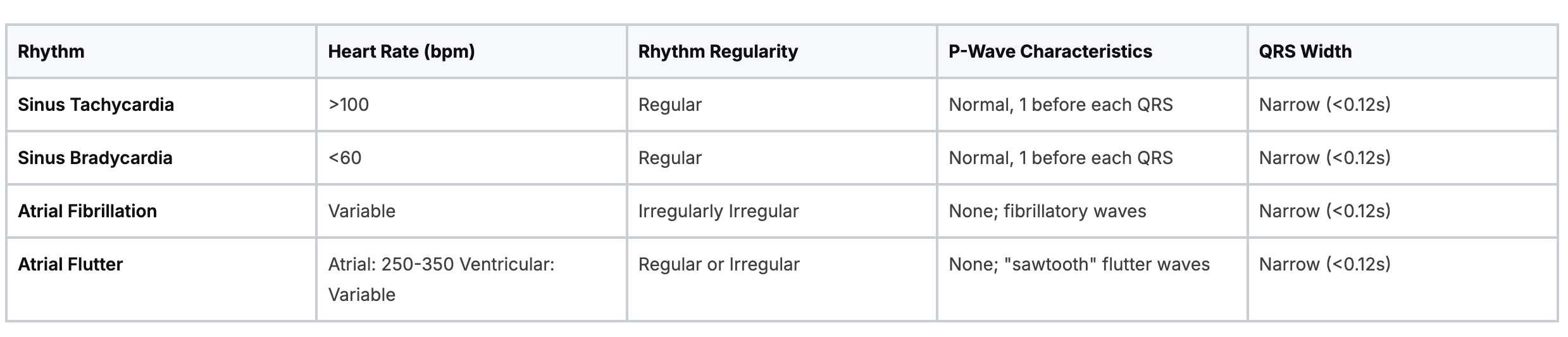
This section is all about building that instant recognition for the usual suspects: Sinus Tachycardia, Sinus Bradycardia, Atrial Fibrillation, and Atrial Flutter. We’ll break down their signature looks on the EKG so you can connect what you see on the screen to the right ACLS algorithm without missing a beat.
Sinus Tachycardia
Think of Sinus Tachycardia as the body’s natural alarm system kicking into high gear. It’s often just a normal response to stress—things like pain, fever, anxiety, or a drop in blood volume. The electrical signal starts in the right place (the SA node), but it's firing way too fast.
On the EKG strip, it looks like a normal sinus rhythm on fast-forward. The dead giveaway is a heart rate greater than 100 beats per minute. Everything else looks perfectly normal: the rhythm is regular, there’s a P wave marching in front of every QRS complex, and the QRS is nice and narrow.
ACLS Perspective: In a code or pre-code situation, the big mistake is treating the number on the monitor. With sinus tach, you don't treat the rhythm itself; you have to play detective and figure out why it's happening. Is the patient bleeding out? Are they in agony? Fix the root problem, and the tachycardia will almost always take care of itself.
Sinus Bradycardia
On the flip side, we have Sinus Bradycardia. This is a rhythm that also starts correctly in the SA node but is just too slow, with a heart rate dipping below 60 beats per minute. Just like its speedy cousin, all the other components are normal: the rhythm is regular, a P wave comes before each QRS, and the QRS is narrow.
Now, this can be totally fine. You'll see it all the time in well-conditioned athletes or even in healthy people while they're sleeping. But in an ACLS scenario, it becomes a major problem if the patient is symptomatic—showing signs that their body isn't getting enough blood, like dizziness, chest pain, or confusion. That's when you have to step in.
Understanding these subtleties is fundamental. A standard EKG paper runs at 25 mm/sec, meaning each tiny box is 0.04 seconds. This little measurement is your key to unlocking everything, from calculating intervals to confirming whether you're dealing with the rapid-fire regularity of sinus tach or the utter chaos of V-Fib. For a deeper look into the nuts and bolts, you can find great resources on ECG interpretation in ACLS.
Atrial Fibrillation (A-Fib)
Atrial Fibrillation, or A-Fib, is one of the most common arrhythmias you will ever lay eyes on. The easiest way to picture it is to imagine the atria (the heart's top chambers) just quivering chaotically, like a bag of worms, instead of giving a good, strong squeeze. This chaotic storm of activity bombards the AV node with hundreds upon hundreds of electrical impulses.
This creates a very distinct, hallmark appearance on the EKG:
- Irregularly Irregular Rhythm: The distance between R waves is completely random and unpredictable. There's no pattern to it whatsoever.
- No Discernible P Waves: Forget about finding neat, rounded P waves. Instead, you'll see a wavy, chaotic, or "fibrillatory" baseline.
- Variable Ventricular Rate: The heart rate can be slow, normal, or dangerously fast, all depending on how many of those chaotic atrial impulses manage to sneak through the AV node.
When A-Fib is paired with a rapid ventricular response (RVR), it's a frequent flyer in ACLS situations because it can quickly cause a patient's blood pressure to tank.
Atrial Flutter
If A-Fib is pure chaos, think of Atrial Flutter as its more organized, but still dangerous, cousin. In this rhythm, a single, hyperactive electrical circuit gets stuck on a loop within the atria, causing them to beat incredibly fast and regularly—often around 300 times per minute. The AV node acts as a gatekeeper, protecting the ventricles by only letting some of these impulses pass through.
The classic, tell-tale sign of Atrial Flutter on an EKG is the "sawtooth" pattern of flutter waves that replace the normal P waves. The ventricular rhythm can be regular or irregular, depending on how consistently the AV node blocks the signals (for example, a 2:1 block, 3:1 block, or a variable block).
Key Characteristics of Common Peri-Arrest Rhythms
To tie all this together and give you a quick-glance reference, this table breaks down the key features of these common peri-arrest rhythms. Use it to solidify the patterns in your mind so you can spot them instantly on a monitor.
Mastering these peri-arrest EKG rhythms for ACLS goes way beyond just passing your certification exam. It's about building the muscle memory and rock-solid confidence you need to act decisively when the stakes are highest.
And remember, this expertise can be built effectively through modern educational formats. Top-tier, accredited online certifications, like those from ProMed Certifications, provide the exact same critical knowledge as in-person classes but with the flexibility, cost-savings, and convenience that today's professionals need. The healthcare industry is evolving, and so is education—ProMed is at the forefront of this change, delivering quality you can trust.
Connecting Rhythms to ACLS Algorithms
Being able to spot a specific EKG rhythm is a crucial skill, but knowing exactly what to do about it is what saves lives. This is where we move from just identifying patterns on a screen to taking decisive action. This section will bridge that gap, turning your EKG knowledge into a real-world playbook for the core ACLS algorithms.
We'll connect each rhythm category to its specific treatment path. Think of it as a roadmap for both mega-code simulations and the chaos of a real emergency.
When a patient is in cardiac arrest, your first look at the rhythm determines which branch of the algorithm you’ll follow. The decision tree starts with one simple question about the heart rate, and that's the first step before you get into the nitty-gritty of the protocols.
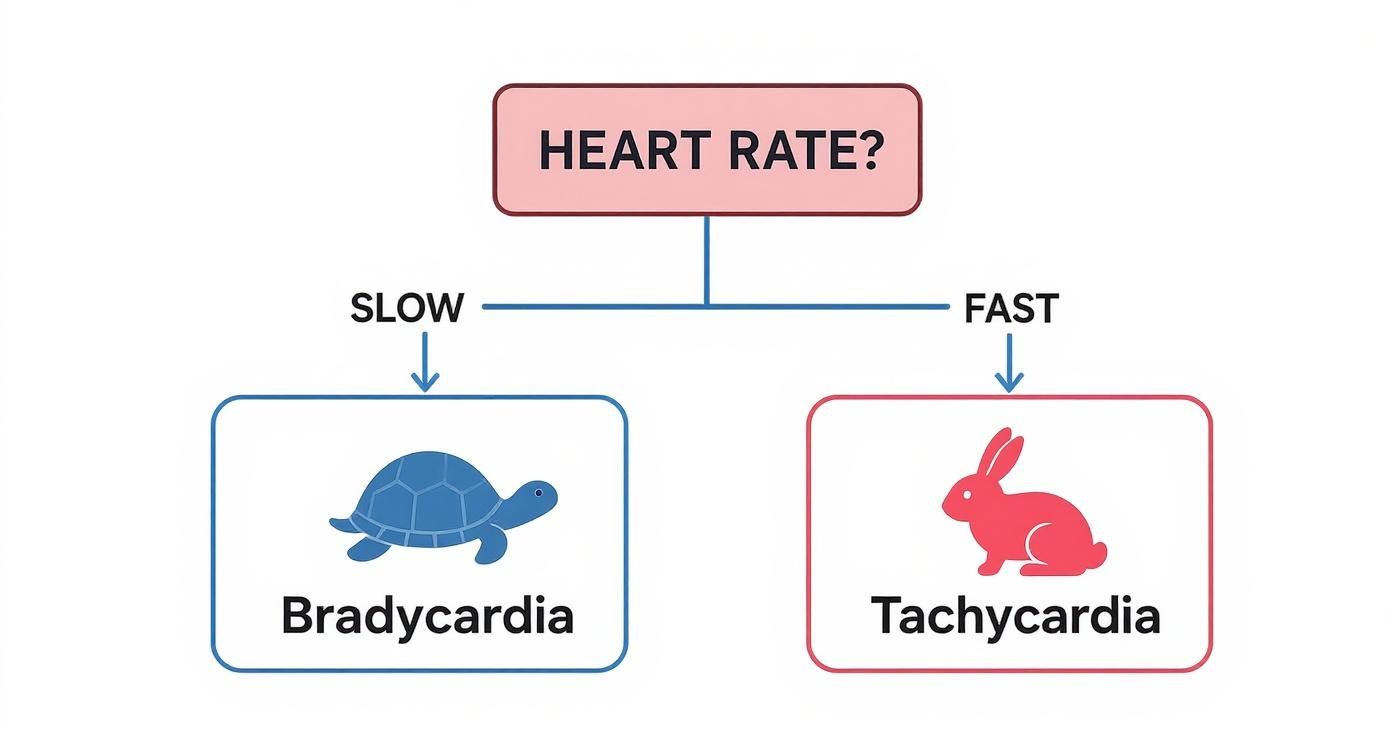
This visual shows that first critical choice: Is the heart rate too slow (bradycardia) or too fast (tachycardia)? For a patient with a pulse, this basic classification points you toward the right ACLS algorithm.
The VFib and Pulseless VTach Pathway
When your monitor screams Ventricular Fibrillation or Pulseles Ventricular Tachycardia, you're on the "shockable" side of the cardiac arrest algorithm. The heart is in a state of pure electrical chaos, and your number one job is to hit the reset button with a high-energy shock.
The sequence is straightforward and every second counts:
- Immediate Defibrillation: The moment that defibrillator is charged, deliver a shock. For biphasic machines, this is typically 120-200 joules.
- High-Quality CPR: Don't waste a second. Right after the shock, get back on the chest for two solid minutes of compressions. No pausing to check the rhythm or pulse. The brain and heart need that blood flow now.
- Rhythm Check and Meds: After two minutes of CPR, take a quick peek at the monitor. If it's still a shockable rhythm, shock again. This is also your window to get IV/IO access and push the first dose of epinephrine (1 mg).
- Antiarrhythmics: If VFib or pVT is stubborn and sticks around after the third shock, it's time to bring in an antiarrhythmic. The go-to choice is amiodarone (300 mg bolus), with a second dose of 150 mg ready if needed.
The Asystole and PEA Pathway
If you see a flatline (Asystole) or organized electrical activity without a pulse (PEA), you've gone down the "non-shockable" side of the algorithm. A shock won't do any good here because there's no chaotic rhythm to reset. The entire game plan shifts to two things: amazing CPR and detective work.
Your priorities are circulation and investigation:
- Uninterrupted CPR: High-quality chest compressions are the only thing creating blood flow. Minimize any and all interruptions.
- Epinephrine Administration: As soon as you have IV/IO access, give 1 mg of epinephrine. Repeat this every 3 to 5 minutes like clockwork. Epi helps constrict blood vessels, which can raise blood pressure and improve flow to the heart.
- Search for Reversible Causes: While CPR is happening, the team needs to be running through the "H's and T's" to find and fix what went wrong. Think Hypoxia, Hypovolemia, Hydrogen ion (acidosis), Tension pneumothorax, Tamponade, Toxins, and the rest.
To see how these pathways all come together, you can review the official Adult Cardiac Arrest Algorithm for a complete visual guide.
Tachycardia and Bradycardia Algorithms
What about patients who are unstable but still have a pulse? ACLS has separate game plans for heart rates that are dangerously fast or slow.
- Tachycardia with a Pulse: If a patient with a rapid rhythm is unstable (think hypotension, altered mental status), the immediate fix is synchronized cardioversion. If they're stable, you have a bit more breathing room to identify the specific rhythm (like SVT or A-Fib) and try medications such as adenosine or other antiarrhythmics.
- Bradycardia with a Pulse: For an unstable patient with a slow heart rate, the first drug out of the box is atropine (1 mg bolus). You can repeat this every 3-5 minutes up to a total of 3 mg. If atropine isn't cutting it, your next moves are transcutaneous pacing or starting a dopamine or epinephrine drip.
Mastering these algorithms means you can look at any EKG rhythm in ACLS and immediately launch into a confident, life-saving response, making sure you give the right care at exactly the right time.
Spotting the Imposters: Common Pitfalls in Rhythm Interpretation
When you're in the middle of a code, the EKG monitor is your lifeline. But that line can sometimes lie. In the heat of the moment, it's dangerously easy to misinterpret a rhythm, and a wrong call can lead you down the completely wrong ACLS path. This is where the real skill comes in—telling the difference between a true lethal arrhythmia and a convincing imposter.
Getting this right isn't just about passing a test; it's about building the rock-solid confidence you need to act decisively, even when the monitor throws you a curveball.
Fine VFib vs. Asystole: The Most Dangerous Look-Alike
This is one of the most critical distinctions you'll ever have to make. A quick glance at a chaotic but very low-amplitude waveform can easily be mistaken for Asystole (a flatline). That split-second decision could lead you to withhold a shock from a patient who desperately needs one.
It’s simple: Asystole is the total absence of electrical activity. Fine Ventricular Fibrillation (VFib) might look weak, but it's still disorganized electrical chaos—and it's absolutely a shockable rhythm.
Before you ever declare a patient is in Asystole, you must run the "Asystole checklist":
- Check the patient: This is always step one. Are they unresponsive with no pulse?
- Crank up the gain: Turn up the amplitude on your monitor. What looked like a flatline might suddenly reveal the subtle, chaotic waves of fine VFib.
- Change your view: Switch to a different lead. A flatline in Lead II might show clear VFib in V1 or another lead.
Never, ever call Asystole based on a single lead. Always confirm it in a second lead and turn up the gain. This simple, two-step check is a foundational rule of ACLS that can literally be the difference between life and death.
The Problem with Artifact
Artifact is the ultimate prankster in emergency medicine. It's any electrical interference that isn't coming from the heart, and it is notorious for mimicking rhythms like VFib or VTach.
What causes it? All sorts of things: a shivering patient, patient movement, loose electrode pads, or even interference from other medical equipment in the room. This can create a terrifying-looking waveform on the screen.
But before you reach for the defibrillator paddles, look at your patient. Are they awake, talking, or moving around? If so, that chaotic mess on the monitor is almost certainly artifact. A quick check to ensure the pads have good contact can often clear it up instantly and prevent a completely unnecessary—and dangerous—intervention.
SVT with Aberrancy vs. Ventricular Tachycardia
Differentiating a wide-complex tachycardia is one of the toughest challenges you'll face. The big question is: are we looking at a Supraventricular Tachycardia (SVT) that's just conducting weirdly (with aberrancy), or is this the much more sinister Ventricular Tachycardia (VTach)?
While there are complex EKG criteria (like Brugada's) to sort this out, in the chaos of a real code, the safest and most effective ACLS approach is simple: assume it's the worst until proven otherwise.
Here are a few quick clues that should immediately make you think VTach:
- How's the patient? If they are unstable—hypotensive, altered, complaining of chest pain—treat it as VTach, period. Don't waste time analyzing subtle EKG features.
- What's their history? A past heart attack (MI), coronary artery disease, or heart failure makes VTach far more likely.
- How wide is it? A QRS complex that's extremely wide (greater than 0.14 seconds) screams VTach.
- Are the P's and QRS's divorced? If you can spot P waves marching along at their own slow, steady pace, completely independent of the wide QRS complexes, that's AV dissociation. It's a slam-dunk sign of VTach.
When you're standing at the bedside with a patient in a wide-complex tachycardia, always err on the side of caution. Treat any regular, wide-complex tachycardia in an unstable patient as VTach. This is the core ACLS principle that keeps patients safe.
The Future of EKG Interpretation and Online Training
Cardiac care is moving fast, and as a medical professional, your education has to keep up. We're seeing game-changing innovations like AI-powered EKG analysis and wearable ECG monitors that are completely changing how we catch and manage critical heart rhythms.
These tools are all about intervening earlier and improving patient outcomes long before a code blue is ever called.
This same forward momentum is happening in medical education. The outdated idea that you can only get a valid certification from an in-person AHA or Red Cross class is quickly becoming a thing of the past. Today, accredited online platforms are leading the charge, offering a modern, evidence-based way to master EKG rhythms in ACLS.
Embracing Evidence-Based Online Learning
Don't just take our word for it. Peer-reviewed study after study has shown that high-quality online training leads to knowledge retention and patient care outcomes that are just as good—and sometimes even better—than traditional classroom settings. Hospitals and clinics get it. They are increasingly recognizing accredited online credentials because they understand it's the quality of the education that matters, not the four walls it's taught in.
This shift isn't happening in a vacuum. Major industry trends are pointing in the same direction. For instance, the market for cardiac rhythm management devices is expected to hit an estimated USD 15 billion by 2034. A huge piece of that growth is remote monitoring, which made up about 39.2% of the ECG band market in 2024. This technology allows for continuous rhythm tracking and much faster identification of arrhythmias.
Choosing an accredited online certification isn't just a matter of convenience. It's about syncing your professional development with the future of medicine and showing a commitment to modern, effective education that gets real-world results.
Platforms like ProMed Certifications are at the forefront of this movement. We provide accessible, credible, and comprehensive ACLS training designed to prepare you for the real challenges of modern cardiac care. By embracing this approach, you're making sure your skills stay sharp and relevant for years to come.
Common Questions About ACLS Rhythms
When you're prepping for a certification exam or, more importantly, standing at the bedside during a code, a few key questions always seem to pop up. Let's tackle some of the most common sticking points when it comes to ACLS rhythms.
How Can I Differentiate SVT With Aberrancy From VTach?
This is the classic dilemma that trips up even seasoned providers. Distinguishing between Ventricular Tachycardia (VTach) and SVT with aberrancy can be tough in the heat of the moment, but a few clues can point you in the right direction.
VTach is the more likely culprit if the patient is unstable, has a history of heart disease, or if that QRS complex is exceptionally wide—think greater than 0.14 seconds. Finding evidence of AV dissociation is another near-certain sign you're looking at VTach.
But here’s the most critical takeaway for ACLS: if you have a regular, wide-complex tachycardia in an unstable patient, you must treat it as VTach until proven otherwise. Hesitation can be fatal, so the safest path is to assume the worst-case scenario and act accordingly.
Why Is CPR So Critical For Non-Shockable Rhythms?
It’s a great question. If a shock resets a chaotic rhythm, why don't we use it for Asystole or PEA? The simple answer is there's nothing to shock.
In Asystole and Pulseless Electrical Activity (PEA), the heart's electrical system has either gone completely silent or it's firing without creating an actual heartbeat. A defibrillator is designed to stop a disorganized electrical storm (like V-Fib or V-Tach) so the heart's natural pacemaker can take over. In PEA and Asystole, there's no storm to stop.
This is where high-quality CPR becomes everything. It's the only thing keeping the patient alive. By manually compressing the chest, you become the heart, forcing oxygenated blood to the brain and vital organs. This critical intervention buys you the precious minutes needed to push drugs like epinephrine and hunt for the reversible causes—the H's and T's.
Are Online ACLS Certifications Accepted By Employers?
Absolutely. The landscape has changed significantly over the past decade. Fully accredited online ACLS certifications are now the standard and are widely accepted by hospitals, clinics, and healthcare systems across the country.
The old stigma against online learning is gone, as institutions now recognize that modern, evidence-based online courses are just as effective—and often more convenient—than traditional classroom settings.
The crucial factor is accreditation. As long as you choose an accredited provider, you can be confident your certification meets national standards and demonstrates the high level of training employers are looking for. It gives you the flexibility your demanding schedule requires without sacrificing quality.
This guide should lay the framework for building your confidence in rhythm interpretation. Mastering ACLS rhythms is a skill that saves lives, and your certification should be just as serious and reliable as your commitment to patient care. At ProMed Certifications, we provide accredited, nationally accepted online courses designed for busy professionals like you.
Get your ACLS certification online with ProMed Certifications today!
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today