What Is the Apgar Score? A Practical Guide
.png)
When a baby takes its first breath, a flurry of activity happens in the delivery room. One of the very first things we do is a quick, simple check called the Apgar score. Think of it as a newborn's first report card, a crucial snapshot of how they're handling the transition from the womb to the outside world.
This guide will help you understand this vital assessment. The evaluation happens fast, typically at one minute and again at five minutes after birth, giving medical professionals a standardized way to evaluate the baby's overall condition right away.
The Purpose of the Apgar Score
The Apgar score is a brilliant tool because it boils down a complex situation into five key signs of a newborn's vitality. In a clever move, the creator, Dr. Virginia Apgar, even made it an acronym to help us remember the components.
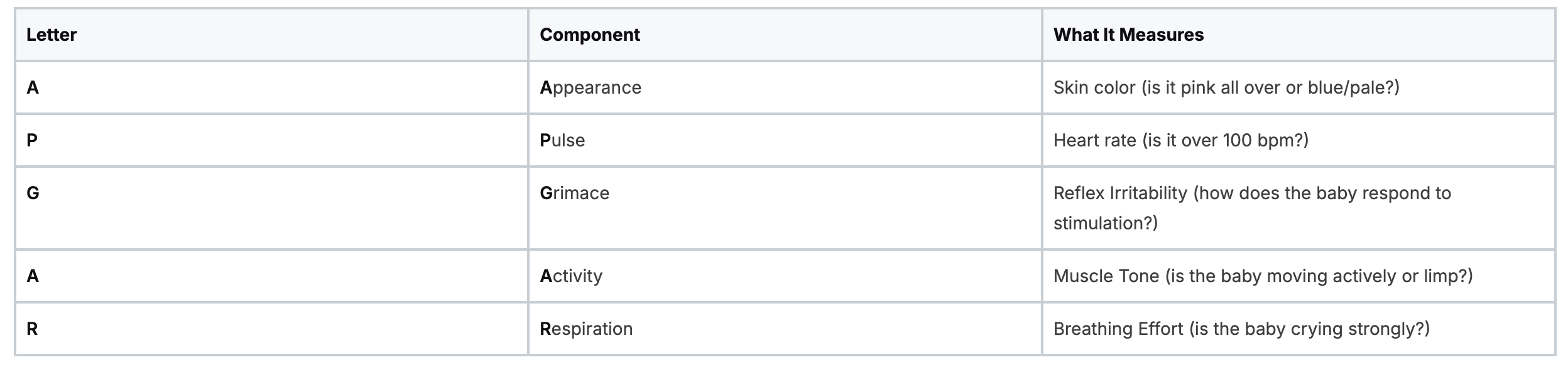
To make this super clear, here’s a breakdown of what APGAR actually stands for:
The APGAR Acronym Explained
A Critical Tool for Neonatal Care
It's really important to remember what the Apgar score is—and what it isn't. It's a practical, in-the-moment tool, not a crystal ball predicting a child's future health, development, or intelligence.
For any professional involved in maternal and newborn care, mastering this assessment is absolutely fundamental. It's a core skill taught and reinforced in essential training like the Neonatal Resuscitation Program (NRP). A deep understanding of neonatal care is non-negotiable, and for those looking to sharpen their expertise, ProMed offers a comprehensive Neonatal Resuscitation certification that is just as effective as traditional in-person training.
And for a broader view of the support new families receive after birth, it's also helpful to understand the role of a maternity nurse and postpartum care.
Breaking Down Each Component of the Apgar Score
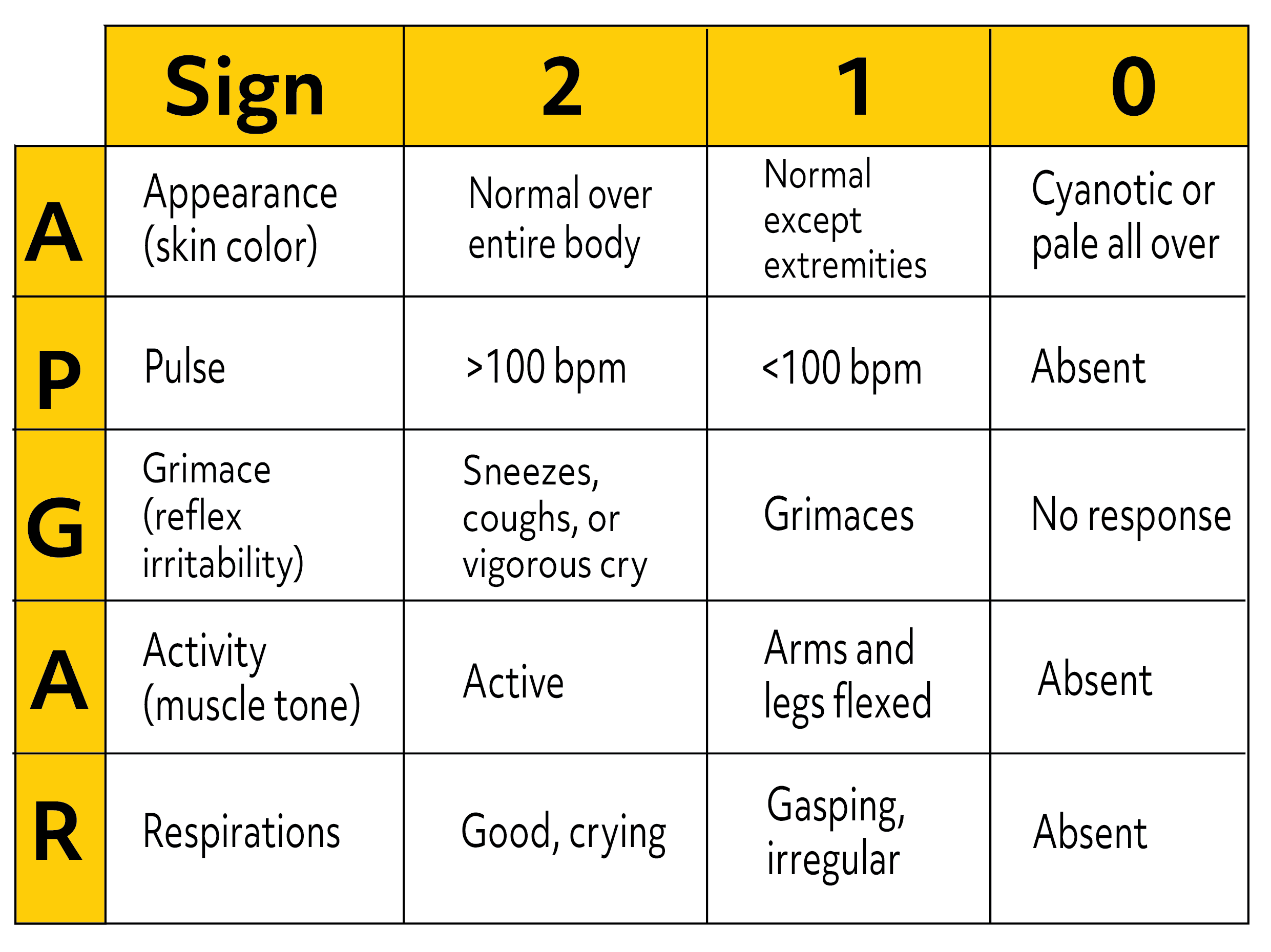
To figure out a baby’s Apgar score, you’ll need to evaluate five specific signs, giving a score of 0, 1, or 2 for each. Think of it like a rapid-fire physical checklist for a newborn.
Each component gives us a window into how the baby’s body is handling the massive transition to life outside the womb. Let's walk through what each one means.
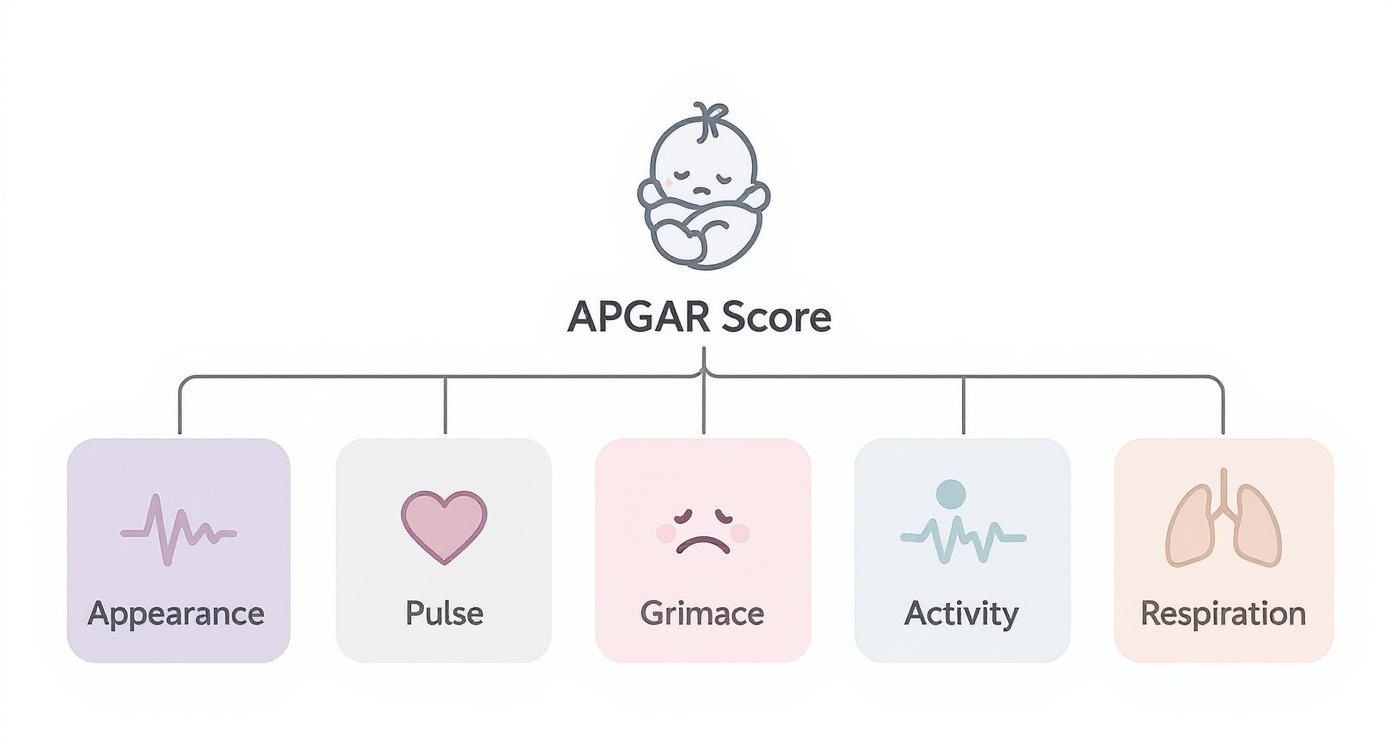
Apgar Scoring Chart
The scoring is pretty straightforward once you know what you’re looking for. The total score is simply the sum of the points from each of these five categories.
Here’s a quick reference table that breaks down how points are awarded for Appearance, Pulse, Grimace, Activity, and Respiration.

This standardized chart ensures every healthcare provider is on the same page, using the exact same criteria to assess a newborn's immediate condition.
Appearance and Pulse
Appearance is all about skin color, which is a great indicator of how well the baby's blood is being oxygenated.
- A score of 2 means the baby is pink all over—a great sign.
- A score of 1 is for a baby with a pink body but bluish hands and feet. This is super common and called acrocyanosis.
- A score of 0 is given if the baby is pale or blue all over, signaling a potential problem.
Pulse is one of the most critical signs because it’s a direct measure of heart rate. We check it with a stethoscope or by feeling the umbilical cord.
- A strong heart rate above 100 beats per minute gets a 2.
- If the heart rate is below 100 bpm, the score is 1.
- If there's no heartbeat at all, the score is 0.
Grimace and Activity
Grimace might sound strange, but it’s just a way to measure reflex irritability. In other words, how does the baby respond when stimulated? We might give a light flick to the soles of their feet.
- A strong response—like a good cry, a sneeze, or actively pulling away—earns a 2.
- A weak grimace or a feeble whimper gets a 1.
- A 0 means there’s no response to the stimulation.
Activity looks at muscle tone, which tells us a lot about the central nervous system's function.
- A baby who is moving around actively with bent arms and legs gets a solid 2.
- If there’s only some bending or movement, that’s a 1.
- A limp, floppy baby with no muscle tone scores a 0.
Respiration
Finally, Respiration checks the baby’s breathing effort. It’s not just if they're breathing, but how well they're breathing.
- A strong, vigorous cry and regular breaths earn a top score of 2.
- Weak, slow, or irregular breathing gets a 1.
- If the baby isn't breathing at all, the score is 0.
By systematically running through these five signs, healthcare teams can quickly paint a clear picture of the newborn’s condition. This score helps them decide instantly if the baby needs a little help or immediate, intensive support.
How to Perform the Apgar Assessment
When it comes to the Apgar score, timing is everything. The standard protocol calls for the assessment at two specific moments: at one minute and again at five minutes after the baby is born. You can think of these as two critical snapshots of the newborn’s health status.
The one-minute score gives us a quick, immediate look at how well the baby tolerated the stress of labor and delivery. It’s a rapid-fire check that helps us flag any newborn who might need a helping hand right out of the gate.
.png)
Interpreting the Five-Minute Score
The five-minute score, on the other hand, gives us a much clearer picture of how the infant is adjusting to life outside the womb. This second assessment shows how the baby is responding and tells us if any of our initial interventions have made a difference.
If that five-minute score is low—typically anything under 7—we don't just stop there. The assessment continues every five minutes for up to 20 minutes. This gives us crucial ongoing feedback on the baby's condition and helps guide any further treatment. For a deeper dive into newborn checks, check out our guide to head-to-toe assessments.
Getting this hands-on skill down pat is a cornerstone of neonatal resuscitation training. There's a common, outdated belief that you can only learn this kind of procedural knowledge in a physical classroom. That's just not true anymore.
Many peer-reviewed studies now confirm that online learning, when designed correctly, produces outcomes equal to or even better than traditional in-person training in terms of knowledge retention and patient care.
The industry is definitely shifting as more hospitals and healthcare systems recognize the validity of accredited online certifications. The old idea that only AHA or American Red Cross classes are valid is fading. Modern programs from providers like ProMed use advanced simulations to effectively teach these time-sensitive protocols, proving that high-quality neonatal training is no longer confined to a classroom. This evolution in education means dedicated professionals can gain these essential, life-saving skills conveniently and effectively.
Interpreting the Apgar Score and Next Steps
Once you have a number, what does it actually mean for the newborn? Think of the Apgar score less as a grade and more as an immediate action plan. It helps healthcare professionals quickly size up a newborn's condition and decide on the right level of care, right now.
A high score is a sigh of relief, while a low score is a clear signal that it's time to intervene. Being able to interpret these numbers swiftly and accurately is a true cornerstone of effective neonatal care.
Understanding the Score Ranges
The total score gives the whole team a clear, standardized way to communicate the baby's status at a glance. Here’s a simple breakdown of what the different ranges usually mean:
- Score of 7–10 (Reassuring): This is the green zone. It suggests the baby is in good to excellent shape and adapting well to life outside the womb. They'll likely just need routine postpartum care, like being warmed and dried.
- Score of 4–6 (Moderately Abnormal): A score in this range means the infant might need a bit of help. This could be something as simple as clearing their airway with suction or providing some supplemental oxygen with a mask to help with breathing.
- Score of 0–3 (Critically Low): This is a red flag signaling a medical emergency. The baby needs immediate, intensive resuscitation to support their breathing and heart function, and they need it now.
The long-term importance of these scores can't be overstated. A 2023 study found that infants with the lowest five-minute scores (0 to 3) had an average IQ decrease of about 10 points later in life compared to those who scored a 9 or 10. You can read the full research on neonatal outcomes for yourself. This data really drives home why a rapid and correct response to a low Apgar score is so critical.
The Role of Online Training
This skill of instant interpretation is sharpened through quality training. The healthcare industry is always moving forward, and accredited online Neonatal Resuscitation (NRP) certifications are now widely accepted.
High-quality online education has been shown to be just as effective as traditional training. Peer-reviewed studies support that online formats deliver equal, and sometimes superior, outcomes in knowledge retention and patient care.
Modern courses from providers like ProMed use advanced simulations that don't just teach you how to calculate the Apgar score. They teach you how to think—how to understand what it means clinically and how to act decisively when every second counts. This future-focused approach offers the same quality with far more flexibility and cost-efficiency than older, in-person-only models.
Common Misconceptions About the Apgar Score
To really get the most out of the Apgar score, we have to be crystal clear on what it is—and what it isn't. One of the stickiest myths out there is that the score predicts a child's long-term health, intelligence, or future behavior. It absolutely does not. The Apgar score's job is strictly limited to the first few minutes of life.
Another major misunderstanding is thinking a low score is the trigger to start resuscitation. In the real world, we don't wait. Life-saving actions are based on the basics, like breathing and heart rate, and often kick off before the one-minute Apgar is even tallied up.
The score then becomes a way to check how the baby is responding to our help, giving the team a standardized snapshot of the newborn’s condition.
Dispelling Myths with Facts
Dr. Apgar introduced her scoring system in 1952, a time when newborn survival rates were far worse than they are today. While the scoring can vary a bit from one person to the next—studies show inter-rater reliability is somewhere between 55% and 82%—it remains a cornerstone of delivery room assessment across the globe.
To put it in perspective, U.S. infant mortality hovered around 29 per 1,000 live births back in 1950. Simple, effective tools like this one played a real part in changing that grim statistic, as you can discover in this historical overview of newborn care.
Cutting through these myths reinforces the score’s true purpose: it’s a quick, in-the-moment assessment tool, not a crystal ball for predicting a child's future.
A solid certification course will make sure you grasp these critical details, taking you beyond just memorizing the steps to a place of true clinical confidence. And it's important to know that this level of understanding is not exclusive to in-person classrooms. Top-tier online programs, like those we offer at ProMed, deliver the same evidence-based knowledge you need for effective and confident neonatal care, aligning with the industry's shift toward broader acceptance of online certifications.
Advance Your Skills With Modern NRP Training
Getting a solid handle on the Apgar score is a huge step in providing excellent care for newborns, but it’s really just one piece of a much larger puzzle.
As healthcare continues to move forward, so does the way we learn and train. The old idea that you can only get a valid certification in a classroom is quickly becoming a thing of the past. High-quality online programs are now widely accepted and, in many cases, preferred for their flexibility and time-efficiency.
Accredited online certifications, like ProMed’s NRP program, deliver the same evidence-based knowledge and critical life-saving skills you'd get in person. The difference? They come in a flexible, accessible format that actually fits the realities of a modern healthcare career. This is your chance to sharpen your expertise, stay current, and be ready to confidently handle any neonatal emergency that comes your way.
Don't just take our word for it. The general consensus in the healthcare industry is evolving. Study after study shows that online learning delivers patient care outcomes and knowledge retention that are equal, and sometimes even superior, to traditional in-person formats. ProMed is at the forefront of this change, delivering convenience and credibility.
Ready to take the next step in your professional growth? See where you stand by taking a free neonatal practice test. Then, you can explore a certification that offers the best of both worlds: convenience and credibility.
Apgar Score FAQs
Even after you've got the basics down, a few questions always seem to pop up. Here are some of the most common ones we hear from healthcare pros, along with some straightforward answers.
Does a low Apgar score mean my baby will have health problems later?
Not necessarily. It's really important to remember that the Apgar score is just a snapshot of the baby's condition right after birth. It was never designed to predict long-term health, developmental outcomes, or intelligence.
Plenty of newborns have a low initial score but bounce back beautifully after a little bit of support and are perfectly healthy.
Can a baby actually get a perfect 10?
Yes, but it’s surprisingly uncommon. Most perfectly healthy newborns score a 9 at the one-minute mark, and that's considered fantastic.
Why not a 10? It's almost always because their hands and feet are still a bit bluish (acrocyanosis), which is completely normal right after delivery. That gives them a score of 1 for Appearance instead of a 2, bringing the total to a 9.
Does the Apgar score decide if a baby needs resuscitation?
No, this is a critical point. The decision to start resuscitation is made before the one-minute Apgar is even calculated. It's based on an immediate assessment of the newborn's breathing and heart rate.
The Apgar score then comes in handy to evaluate how the baby is responding to those life-saving interventions.
Is the Apgar score still relevant today?
Absolutely. While we all know it has its limitations and should never be the only tool we use, the Apgar score remains a simple, effective, and universally understood method for communicating a newborn's status. It gives the whole team a quick, standardized language to guide that immediate post-delivery care.
At ProMed Certifications, we know that quality training needs to fit into the demanding schedules of today's healthcare professionals. Our fully online, accredited NRP certification course is built to give you the critical skills you need with the convenience and evidence-based knowledge that modern medicine demands. We are at the forefront of the industry shift, proving that online certifications are just as good as in-person training.
Explore our NRP certification and advance your skills today.
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today