How to Read EKGs for Dummies: a Beginner's Guide

When you first lay eyes on an electrocardiogram (EKG or ECG) strip, it can look like an intimidating mess of squiggles. But those lines tell a vivid story about the heart's electrical system, and learning to read them is a skill anyone in the medical field can master—not just cardiologists.
Think of an EKG as a seismograph for the heart. It doesn’t show you how well the heart is physically pumping blood, but it does capture the electrical impulses that make it pump. It's all about understanding that story, one beat at a time. This guide will help you build a solid foundation so you can interpret EKGs with confidence.
The Anatomy of a Single Heartbeat
At the core of EKG interpretation is recognizing a simple, repeating pattern. Every single heartbeat creates a predictable waveform with three main parts. Getting these down is your first, most important step.
You're essentially looking for the P wave, the QRS complex, and the T wave. Think of it as a three-act play that repeats with every beat, showing you exactly how electricity is traveling through the heart.
- P Wave: This is that first small, rounded bump. It shows us atrial depolarization—the electrical spark that makes the atria (the heart's top chambers) squeeze.
- QRS Complex: This is the big, spiky part that jumps off the page. It represents ventricular depolarization, the much more powerful signal that causes the ventricles (the bottom chambers) to contract and push blood out to the body.
- T Wave: Following the spike is a more modest, rounded hill. This is the T wave, and it signals ventricular repolarization. This is the moment the ventricles electrically reset, getting ready for the next beat.
Nailing these three elements—P, QRS, and T—is the foundation for everything else you'll learn.
Why Do We Need 12 Different Views?
You've probably heard the term "12-lead EKG" and wondered, why so many? A standard 12-lead EKG uses 10 electrodes placed on the patient's chest and limbs to generate 12 different electrical "pictures" of the heart from various angles.
It’s like setting up a dozen cameras around a building to get a complete 360-degree view. Each camera—or lead—gives you a unique perspective. Some look at the front of the heart, some the side, and others the bottom.
This multi-angle view is crucial for diagnostics. It helps us pinpoint the exact location of a problem, like ischemia or a full-blown heart attack (myocardial infarction). While this guide will focus on interpreting basic rhythm strips (usually from a single lead), knowing that a 12-lead EKG provides a much more comprehensive picture is key context for your learning journey.
A Systematic Approach to Reading Any EKG
The real secret to confidently reading an EKG isn't about memorizing hundreds of bizarre-looking rhythm strips. It’s much simpler than that. It's about developing a consistent, step-by-step method you stick to every single time, without fail. Following a reliable sequence prevents you from glossing over subtle but critical clues, turning what feels like a guessing game into a methodical, reliable skill.
Sticking to a process ensures you evaluate every single part of the cardiac cycle. Think of it as your best defense against misinterpretation, especially when the pressure is on. The hard truth is, competency in reading EKGs is often much lower than you'd expect. With over 300 million EKGs performed every year in hospitals, clinics, and ambulances, having a rock-solid system isn't just a good idea—it’s essential for patient safety.
A 2022 study really put a spotlight on this issue. It found that among 325 medical professionals and students, the average competency score was a shocking 5.13 out of 10. Even more concerning, over 77% couldn't correctly identify a normal sinus rhythm, which is the most fundamental pattern there is. The best way to close that gap and build real confidence is to adopt a structured approach from day one.
The Foolproof EKG Checklist
Consider this your pre-flight checklist before making any clinical decision based on an EKG. Working through these points in order builds a routine that ensures nothing important gets missed.
- Rate: First things first, what's the heart rate? Is it fast (tachycardia), slow (bradycardia), or sitting in that normal range of 60-100 bpm?
- Rhythm: Next, is the rhythm regular or irregular? Look at the R-R intervals—are they consistent, or are they all over the place?
- P Waves: Now, zoom in on the P waves. Are they even there? Do they all have the same shape? And critically, is there one P wave for every QRS complex?
- PR Interval: Measure the time from the start of the P wave to the beginning of the QRS. A normal PR interval is between 0.12 and 0.20 seconds. Is it too long, too short, or just right?
- QRS Complex: Analyze the QRS complex. Is it narrow (less than 0.12 seconds) or wide? This is a huge clue about where the electrical impulse is starting from.
- QT Interval & T Waves: Finally, check out the QT interval and the shape of the T waves. Funky-looking T waves or a prolonged QT can point to things like electrolyte imbalances or even ischemia.
This image helps visualize the key waves and complexes you'll be scrutinizing as you work through your checklist.
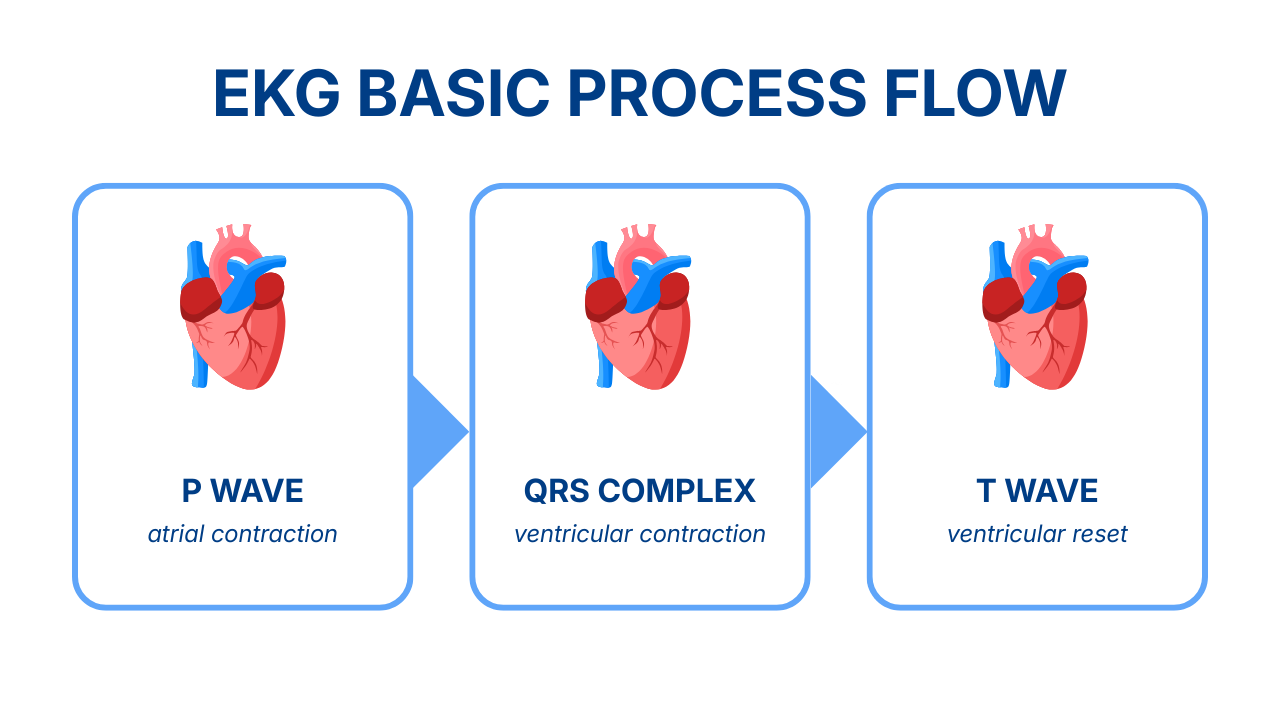
It perfectly illustrates the anatomy of a single heartbeat: the P wave (atrial contraction), the QRS complex (ventricular contraction), and the T wave (ventricular reset).
For a quick reference, here are the normal values you'll be comparing your findings against.
Normal EKG Interval and Waveform Values
This table is your go-to cheat sheet for standard measurements. As you work through your EKG analysis, you can quickly reference these values to see if anything is out of the ordinary.
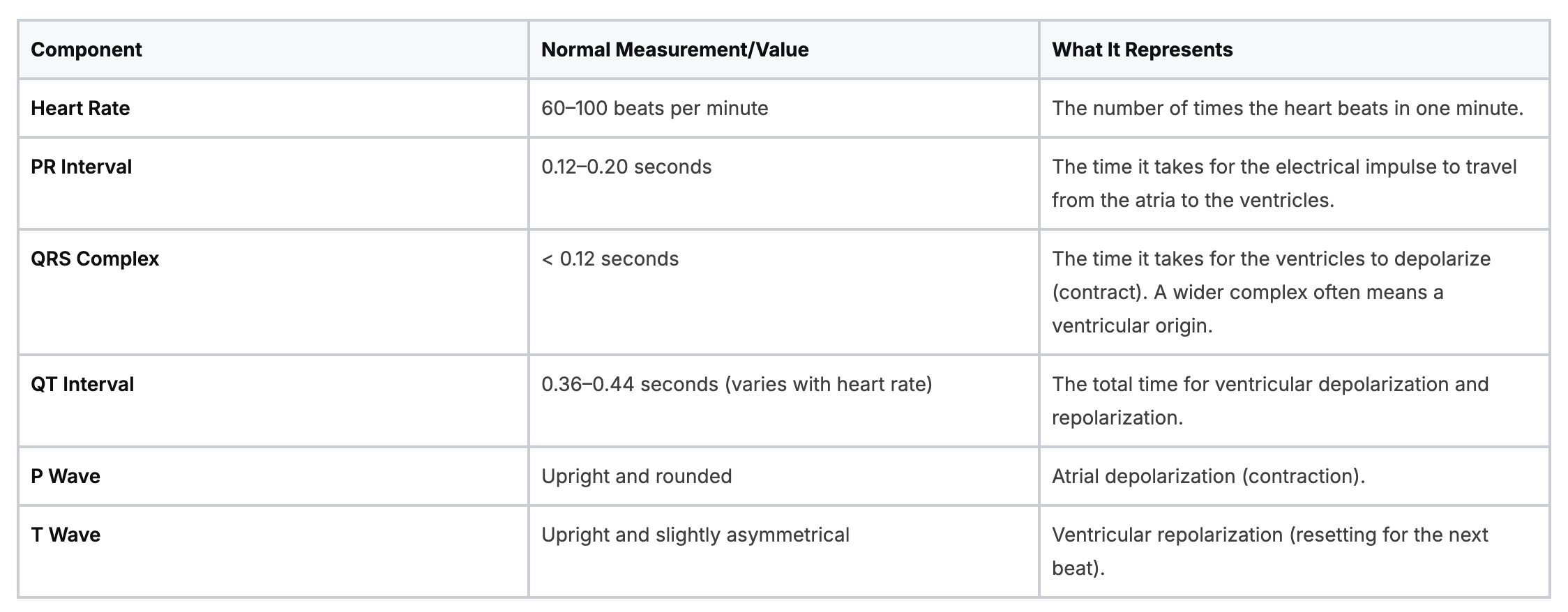
Keep these numbers handy. Soon enough, you won't even need to look them up.
Quick Tricks For Calculating Heart Rate
Calculating the heart rate is always your first step, and thankfully, you don't need a calculator. There are a couple of quick-and-dirty methods that work great.
The 6-Second Strip Method
This is by far the easiest and most reliable trick, and it's my go-to for irregular rhythms. Most EKG strips have small hash marks at the top or bottom indicating 3-second intervals.
- Find a 6-second portion of the strip (two of the 3-second sections).
- Count the number of QRS complexes you see in that window.
- Multiply that number by 10.
Simple as that. If you count 8 QRS complexes in your 6-second strip, the heart rate is about 80 beats per minute (8 x 10 = 80).
The 300 Method
This one is lightning-fast but really only works well for regular rhythms. It’s a great way to get a quick estimate.
Find an R-wave that lands perfectly on a heavy black line on the EKG grid. From there, count down for each subsequent heavy line: 300, 150, 100, 75, 60, 50. Wherever the next R-wave lands is your approximate heart rate.
If the next R-wave hits the very next heavy line, the rate is 300 bpm. If it's two lines over, it's 150 bpm, and so on.
The Value Of Consistent Training
Mastering this systematic approach all comes down to one thing: practice. The more strips you analyze using this checklist, the faster and more intuitive it becomes. This foundation is non-negotiable before you start trying to tackle more complex arrhythmias. To keep building your skills, check out our basic guide to ACLS ECG interpretation, which takes a deeper dive into rhythm analysis.
The goal is to make this process second nature. Every single time you pick up an EKG, you should automatically start with rate, then rhythm, then P waves, and on down the line. That consistency is what separates a novice from a seasoned pro and, most importantly, leads to better, safer patient care.
Identifying Common Cardiac Arrhythmias
Once you've got a solid, systematic approach down, you get to the exciting part: recognizing abnormal heart rhythms. This is where all that foundational knowledge clicks into place and becomes a real-world, life-saving skill. It’s like you've learned the alphabet, and now you’re finally starting to read. We're going to dive into the most common and critical arrhythmias you’ll see in any clinical setting.
Unfortunately, getting these interpretations wrong is more common than you'd think. A 2023 study in PLOS One really drove this point home. Researchers surveyed 231 emergency medical professionals and found their average accuracy in identifying 12 common EKG rhythms was a shockingly low 43.3%.
What's more, over 74% couldn't spot critical findings like pathological Q waves, which can be a dead giveaway of a previous heart attack. This is a sobering reminder that pattern recognition is a skill that demands constant practice and a sharp eye.
The Must-Know Tachycardias
When the heart starts racing (tachycardia), it's usually because of an electrical glitch starting in either the atria or the ventricles. These are the big ones you absolutely have to know on sight.
- Atrial Fibrillation (A-Fib): The classic sign of A-Fib is an "irregularly irregular" rhythm. The R-R intervals are all over the map, and you won't find any clear P waves. All you'll see is a chaotic, wavy baseline.
- Atrial Flutter: Look for the unmistakable "sawtooth" pattern of flutter waves where the P waves should be. The ventricular response can be regular or irregular—it just depends on how many of those rapid-fire signals make it through the AV node.
- Premature Ventricular Contractions (PVCs): You’ll see a run of wide, bizarre-looking QRS complexes (>0.12 seconds) at a rate that's typically over 100 bpm. P waves are usually lost in the chaos. V-Tach can be stable (with a pulse) or unstable (pulseless) and can spiral into V-Fib in a heartbeat.
- Ventricular Fibrillation (V-Fib): It's pure chaos. V-Fib is a disorganized, messy squiggle with no identifiable waves or complexes at all. If you see this, there is no pulse.
Understanding Bradycardias and Heart Blocks
Just as a fast heart can spell trouble, a slow one (bradycardia) can be just as dangerous. This is often caused by a "heart block," where the electrical signal gets delayed—or completely stopped—on its journey from the atria to the ventricles.
Think of the AV node as a gatekeeper between the atria and ventricles. In heart blocks, this gatekeeper is either slow, unreliable, or completely closed for business.
- Sinus Bradycardia: The only thing you'll see is a prolonged PR interval (>0.20 seconds) that stays the same from beat to beat. Everything else about the rhythm looks normal.
- Second-Degree Atrioventricular (AV) Block - Mobtiz Type I: The pattern is the key: "longer, longer, longer, drop!" It’s a classic, repeating sequence that's easy to spot once you know what you're looking for.
- Second-Degree Atrioventricular (AV) Block - Mobitz Type II: You’ll see P waves marching along with consistent PR intervals, but some P waves will have no QRS after them. Mobitz II is notorious for progressing to a complete heart block without warning.
- Third-Degree Atrioventricular (AV) Block aka Complete Heart Block.: You'll see no relationship whatsoever between the P waves and the QRS complexes. The atria march along at their own rate, and the ventricles beat to their own, much slower, escape rhythm.
Learning to spot these common arrhythmias is a huge step in your journey. The more strips you look at, the faster these patterns will start to jump out at you.
Spotting Myocardial Ischemia and Infarction
Beyond just rhythm problems, the EKG is your frontline tool for catching one of the most time-sensitive emergencies you'll ever face: a heart attack, also known as a myocardial infarction (MI). Learning to spot the tell-tale signs of a heart starved for oxygen (ischemia) or one that is actively dying (infarction) is a non-negotiable skill. This is where your ability to read an EKG can genuinely change a patient's life.
When a coronary artery gets blocked, the heart muscle it feeds begins to suffer. This stress and injury at the cellular level creates distinct, recognizable changes on the EKG tracing. Your job is to find these changes fast and know exactly what they mean.
The Three Big Clues of Ischemia and Infarction
While there are plenty of subtle signs, three major EKG changes practically scream "cardiac emergency." If you're just starting out, these are the ones to burn into your memory.
- ST-Segment Elevation: This is the classic sign of an acute, full-thickness heart attack called a STEMI (ST-Elevation Myocardial Infarction). The J-point, where the QRS complex ends, gets pulled upward, making the whole ST segment look elevated. A STEMI is a true medical emergency that requires immediate intervention.
- ST-Segment Depression: When you see the ST segment dipping below the baseline, it's often a red flag for myocardial ischemia. This means the heart muscle isn't getting enough oxygen, but irreversible damage might not have happened yet. Think of it as a serious warning shot that a major event could be right around the corner.
- T-Wave Inversion: Flipped T-waves can also point to ischemia. If T-waves that are normally upright suddenly point downward in specific leads, it suggests a lack of blood flow to that area of the heart.
Catching these changes is absolutely critical for patient outcomes. A 10-year analysis of over 342,000 patients showed that even subtle abnormal T-waves can independently predict mortality. Yet proficiency is a real issue. An NIH study involving 1,024 professionals found the average interpretation score was just 56.4%. Unsurprisingly, the data showed that those who read more EKGs and had more training performed significantly better.
Pinpointing the Location of the Problem
A 12-lead EKG is brilliant because it doesn't just tell you if there's a problem; it helps you figure out where the problem is. Think of the leads as little cameras pointed at different walls of the heart. By seeing which leads show ST elevation or depression, you can localize the injury.
This is a fundamental concept you'll build on. For example, if you see ST elevation in leads II, III, and aVF, you're looking at an inferior wall MI. Changes in leads V3 and V4, on the other hand, point straight to an anterior wall MI.
A Pro Tip on Confirmation: Reciprocal Changes
When one wall of the heart is injured and shows ST elevation, the leads viewing the opposite wall often show ST depression. These are called reciprocal changes, and they're a powerful way to help confirm your diagnosis of a STEMI.
Tying It All Together with Clinical Context
Always remember, the EKG is just one piece of the puzzle. You have to interpret it within the context of what's happening with the patient. A patient with crushing chest pain whose EKG shows clear ST elevation is a completely different scenario than an asymptomatic patient with some non-specific T-wave changes.
Never treat the EKG; treat the patient. The tracing gives you vital clues, but your clinical judgment is what ultimately guides your actions. Mastering these patterns will take you from someone who just looks at EKGs to a clinician who truly understands what they're saying.
Why Online Certification is the Modern Standard
Reading a guide like this is a fantastic first step, but to really nail EKG interpretation, you need certified training and a whole lot of practice. In the past, that meant giving up a weekend for a stuffy, in-person class. Thankfully, medical education has caught up with the times, and high-quality online certification has become the go-to for busy healthcare professionals.
There's an outdated belief that only in-person courses from organizations like the American Heart Association or the American Red Cross are valid. This is simply no longer true. The healthcare industry is widely recognizing the value and effectiveness of accredited online continuing education (CE) and certifications.
The Shift Toward Flexible and Effective Learning
Modern healthcare doesn’t punch a clock from 9-to-5, so why should your education? The move to online learning isn't about finding shortcuts; it's about meeting the real-world demands of clinicians with a format that actually respects their time and improves how they learn. Accredited online providers offer a potent alternative that fits right into a packed schedule.
This isn't just a trend; it's backed by a growing mountain of evidence. Many peer-reviewed studies have shown that online learning is just as effective—and sometimes even better—than traditional classroom settings. These studies consistently show that outcomes for patient care, knowledge retention, and learner flexibility are equal or superior in online formats:
- Knowledge Retention: Self-paced modules let you digest complex topics like EKG interpretation on your own terms, which leads to much better long-term recall.
- Learner Flexibility: You can study whenever and wherever it works for you, whether that's during a quiet moment on a night shift or in between patient appointments.
- Improved Patient Outcomes: When education is this accessible, professionals are far more likely to stay sharp and current with the latest guidelines. That directly translates to better patient care.
Platforms like ProMed Certifications are at the forefront of this change. We built our entire platform on the idea that top-tier education should be both credible and convenient. Our courses deliver the same high-caliber training you’d expect from any major institution, but with practical benefits that fit your life—like cost savings, time efficiency, unlimited exam retakes, and instant, lifetime access to all your materials.
Why Hospitals and Clinics are Embracing Online Certifications
The acceptance of online certifications by healthcare employers is growing every single day. Hospitals, clinics, and regulatory bodies now recognize that the quality of your education is defined by the curriculum and accreditation—not the building you learned it in. They get that a well-designed online program can offer a rigorous and highly effective learning experience.
The industry consensus is slowly shifting: a certification's validity now hangs on its adherence to the latest ILCOR and AHA guidelines and its accreditation status, not on whether you sat in a specific classroom.
This is exactly why ProMed Certifications offers a full money-back guarantee. We're confident that our accredited ACLS, PALS, and BLS certifications will be accepted by your employer. When you choose a quality online program, you're investing in a future-focused way of learning that gives you both the skills you need and the credentials you can count on. It's a smarter, more efficient way to advance your EKG interpretation skills without having to put your career or life on hold.
Burning Questions About EKG Interpretation
Jumping into the world of EKGs always stirs up a lot of questions. As you start trying to apply what you've learned to actual strips, you'll find that everyone hits the same few roadblocks. Let's clear up some of the most common questions to help you get unstuck and build some real confidence.
Think of this as tying up the loose ends. Once these common points of confusion are sorted out, your systematic approach will feel much more natural and effective.
How Long Does It Really Take to Learn This?
This is the big one, and the honest-to-goodness answer is: it depends. You can get the hang of basic rhythm recognition in just a few solid study sessions. Soon enough, you'll be able to spot major troublemakers like A-Fib or V-Tach without much trouble.
But getting really good? That's a different story. True proficiency—the kind where you can confidently interpret a complex 12-lead EKG and catch all the subtle clues—is a skill you build over months and years of consistent practice. It's less about cramming facts and more about making your systematic approach an ingrained habit for every single strip you see.
Do You Have to Be a Cardiologist to Read an EKG?
Absolutely not. While cardiologists are the undisputed experts, reading EKGs is a must-have skill for a huge range of healthcare pros—nurses, paramedics, PAs, and ER docs, just to name a few. The level of detail you need to master really depends on your role.
A paramedic's priority is spotting life-threatening rhythms in seconds. A primary care provider, on the other hand, might be looking for hints of chronic conditions or ischemia during a routine check-up. Your goal is to become an expert at the level your job demands so you can provide the right care at the right time.
A lot of people think EKG interpretation is some kind of exclusive, high-level skill. The truth is, it's a core competency that helps clinicians at every level make smarter, faster decisions for their patients.
What are the Most Common Beginner Mistakes?
When you're starting out, it's easy to fall into a few common traps. Just knowing what they are is half the battle in avoiding them.
- Ditching the System: The single biggest mistake is jumping to conclusions. You see a wide QRS complex and your brain screams "V-Tach!"—but you forgot to check the rate, the underlying rhythm, or look for P waves. That's how serious errors happen. Stick to your checklist, every single time.
- Forgetting the Patient: An EKG strip is just a piece of paper (or a screen). It isn't a diagnosis. ST elevation doesn't mean anything without the context of a patient complaining of crushing chest pain. Always, always connect what you see on the strip to the person in front of you.
- Getting Tunnel Vision on One Lead: One lead is just one snapshot of the heart. What looks like a big deal in a single lead might be nothing to worry about when you look at the others. This is especially critical when you're working with a full 12-lead EKG.
Is Online EKG Training Actually Any Good?
Yes, without a doubt. There's an outdated mindset that says you can only get a valid medical certification from an in-person, AHA or Red Cross class. That is simply not the case anymore. The healthcare world has widely accepted that high-quality, accredited online education is every bit as effective as sitting in a classroom.
Many peer-reviewed studies and industry articles have demonstrated that when it comes to retaining knowledge and improving patient care, online courses are on par with—and sometimes even better than—traditional methods. They give you the flexibility to learn at your own pace, which is a huge advantage for a complex topic like EKG analysis. As long as the training provider is accredited and follows the latest ILCOR and AHA guidelines, your certification is legitimate and will be recognized.
This guide should give you a solid framework for building your EKG interpretation skills. The real work begins when you put this knowledge into practice with certified training. ProMed Certifications offers fully accredited online courses that are guaranteed to be accepted, letting you master this vital skill on a schedule that works for you.
.avif)
Stay compliant with ProMed+
Certifications included: ACLS, BLS, PALS, CPR & Neonatal Resuscitation
Unlimited continuing education: over 200 hours of accredited CME
All-inclusive: One price. No surprises.
Get certified today